Immune checkpoint inhibitors in metastatic melanoma therapy (Review)
- Authors:
- Published online on: February 9, 2024 https://doi.org/10.3892/mi.2024.137
- Article Number: 13
-
Copyright : © Shah et al. This is an open access article distributed under the terms of Creative Commons Attribution License [CC BY 4.0].
Abstract
1. Introduction
The incidence of melanoma has increased over the past two decades (1). Each year, melanoma affects more than 325,000 people. Males experience more frequent occurrences, with 174,000 yearly cases compared to females, with 151,000 cases (2). Of note, 20% of patients with melanoma eventually develop unresectable or distant metastatic disease labeled as stage III/IV (3). Unfortunately, for such an advanced-stage disease, the prognosis remains bleak. However, understanding the advanced stages of melanoma growth and progression has led to the development of promising new therapeutic alternatives.
Until 2011, chemotherapy was the initial treatment for metastatic melanoma; however, it only provided a 6-month median survival time and a 25% 1-year overall survival rate. High-dose interleukin-2 (IL-2) was the only immunotherapy available, but was associated with severe toxicities and only benefited a limited number of patients (4). Currently, advances in immunotherapy and studies on cell cycle regulatory molecules have facilitated the creation of immune checkpoint inhibitors (ICIs), a group of monoclonal antibodies that block co-inhibitory molecules, such as cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4), programmed cell death protein 1 (PD-1) and its ligand, PDL1 (5-7). Ipilimumab, nivolumab and pembrolizumab were the first class of medications shown to improve the overall survival of patients with metastatic melanoma (4).
The present review provides comprehensive evidence regarding the role of ICIs and their utilization in advanced melanoma cases. The outcomes of ICIs, such as ipilimumab, nivolumab and pembrolizumab are highlighted, including the improved survival rates and response rates associated with their use compared to traditional chemotherapies, while also focusing on the mechanisms and demonstrating the potentially adverse effects of these therapies.
Furthermore, the present review focuses on combination therapies, including anti-PD1 with anti-CTLA-4, showcasing their importance compared to monotherapy. The improved outcomes of combination therapies over traditional therapies are highlighted, with an emphasis on the need for ongoing research, optimized treatment approaches and strategies which can be used to overcome resistance. In addition to discussing the development of novel biomarkers for assessing ICI therapeutic responses in both tissue and serum-based prognostic and predictive markers, tumor metabolic dependencies and targeting the metabolic pathways by combining ICIs are also discussed. This could provide an improved efficacy, which, to the best of our knowledge, has not been described commonly in the available literature focusing on ICIs used in melanoma.
2. Immune checkpoint inhibitor drugs and their role in metastatic melanoma
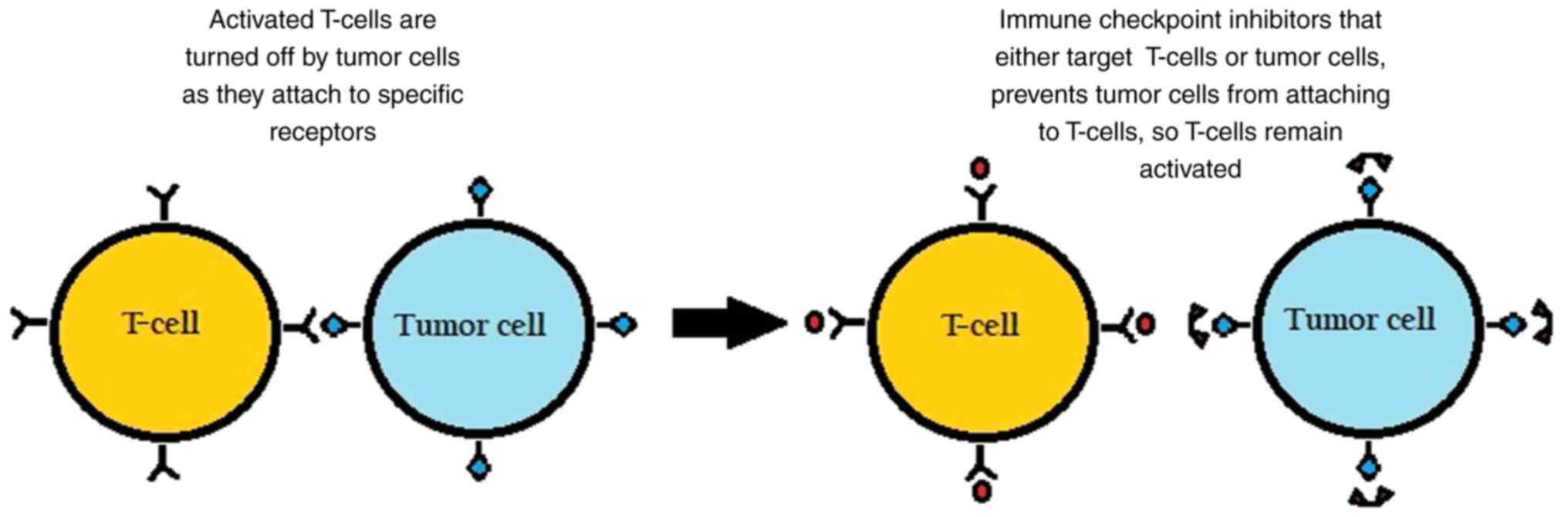
The surface of immune cells, such as T-cells, assists in the regulation of the immune response through various receptors. When activated by certain ligands, these receptors inhibit immune cells from attacking the body's own cells. However, in cancer, tumor cells can take advantage by binding to these checkpoint-inhibitory receptors through their own ligands and suppressing the immune response, as illustrated in Fig. 1.
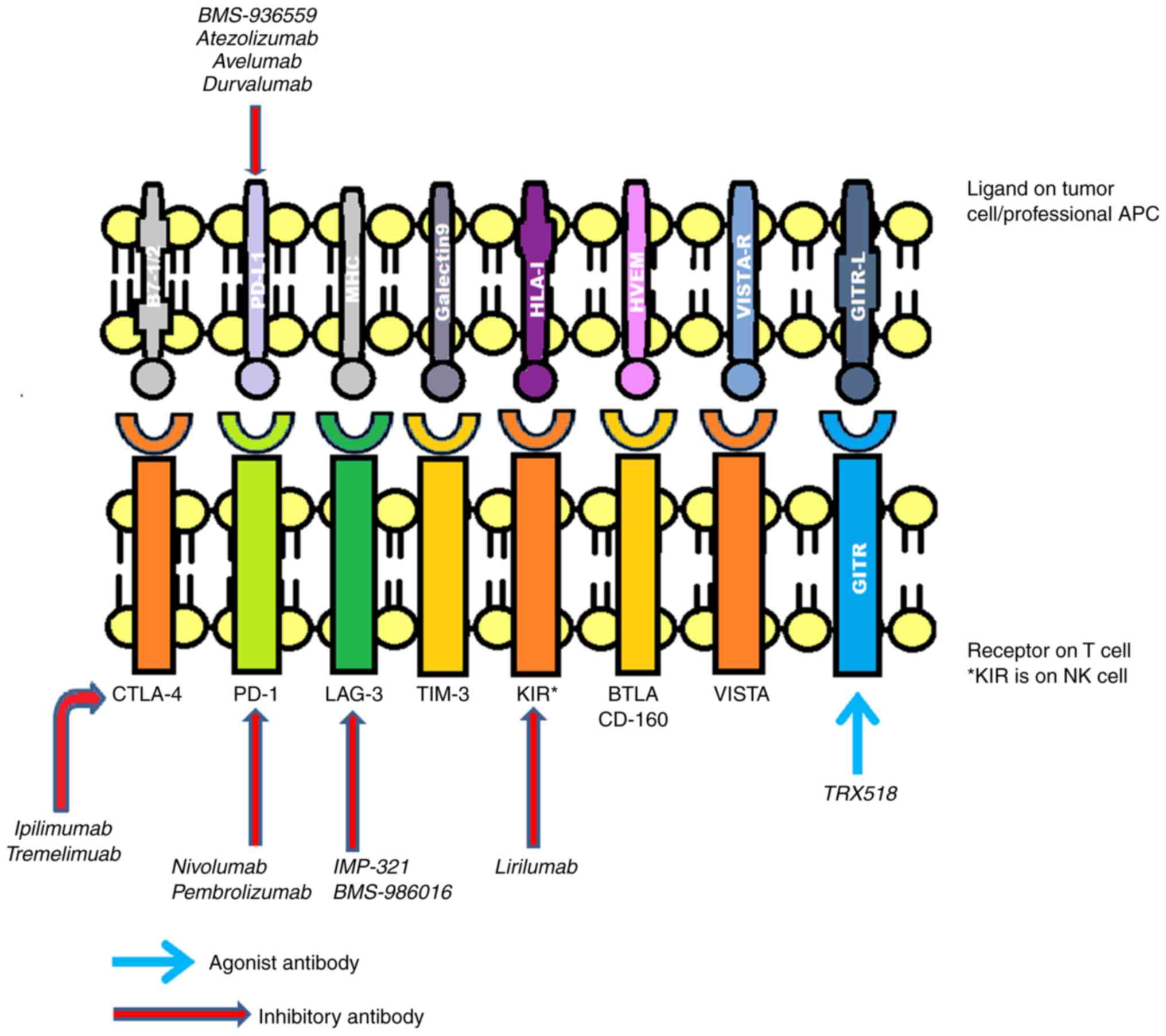
Commonly implicated inhibitory receptors include (CTLA-4, PD-1, T-cell immunoglobulin domain and mucin domain-3 (TIM-3), killer cell immunoglobulin-like receptor (KIR), lymphocyte-activation gene 3 (LAG3), glucocorticoid-induced tumor necrosis factor receptor (GITR), B- and T-lymphocyte attenuator (BTLA) and V-domain immunoglobulin (Ig)-containing suppressor of T-cell activation (VISTA) (8-10), as presented in Fig. 2.
Over time, several drugs have been introduced targeting these receptors. Ipilimumab was one of the first ICI drugs to be approved by the Food and Drug Administration (FDA) for the treatment of metastatic melanoma, which functions by blocking CTLA-4(11). There are numerous additional comparable drugs in early phase III, phase II, or preclinical research. These include pidilizumab, atezolizumab, durvalumab and tremelimumab (formerly known as ticilimumab) (12,13). To increase the immune system's defense against cancer cells, these medications also work against various immunological checkpoints (12,13).
3. Mechanisms underlying the effectiveness of ICIs in metastatic melanoma
CTLA-4 and anti-CTLA-4 drugs
CTLA-4, a B7/CD28 family member, is a coinhibitory receptor expressed on the surface of T-cells that eventually inhibits T-cells, and it is expressed by regulatory T-cells (Tregs) (14). Discovered in 1987, it was considered to function as a negative regulator of T-cell activation until the mid-1990s (15-17).
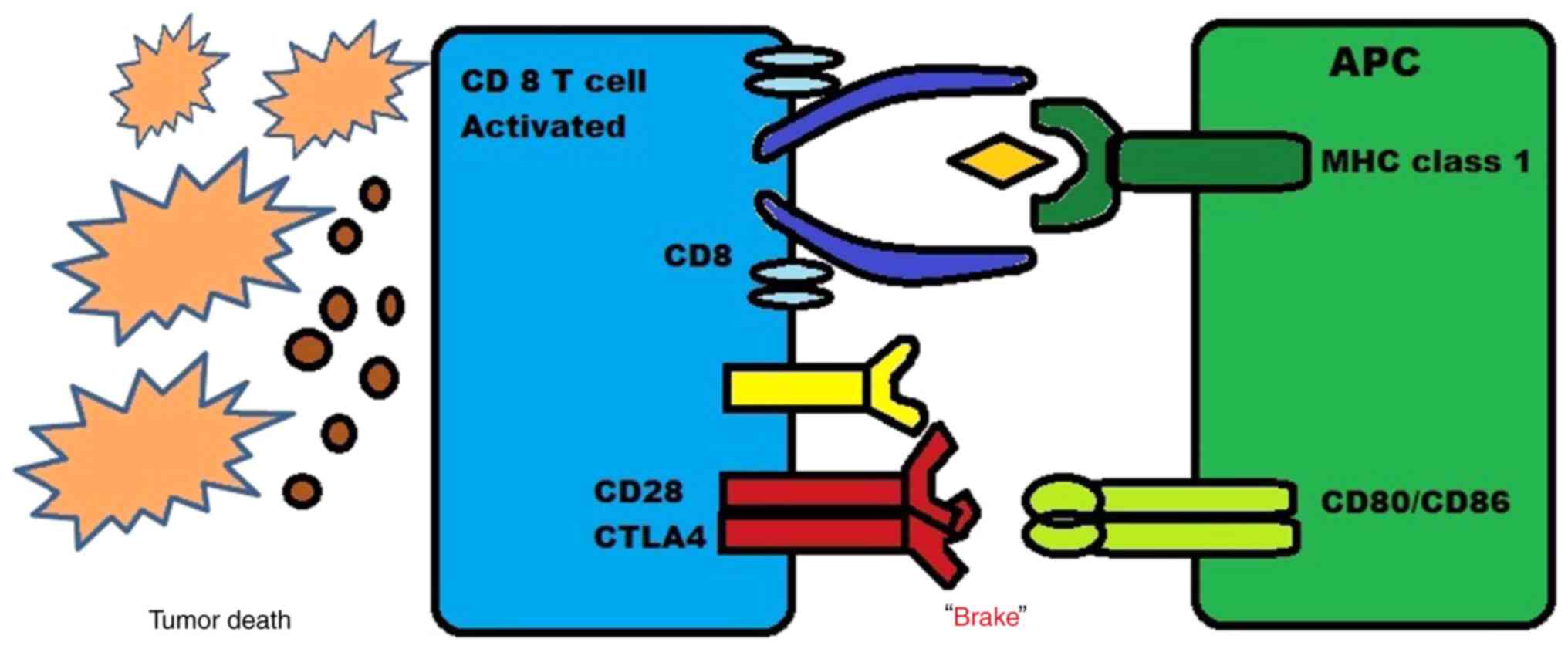
When CTLA-4 is expressed on the surface of CD4+ and CD8+ T-cells, the binding affinity increases and is higher to CD80 and CD86, which are the costimulatory receptors present on antigen-presenting cells (APCs) compared to CD28 which is another costimulatory receptor (18). The expression of CTLA-4 increases when there is an activation of T-cell receptors and the release of cytokines such as IL-12 and interferon (IFN)-γ. This upregulation creates a feedback inhibition loop on T-effector cells which are activated, leading to CTLA-4 acting as a natural ‘brake’ on CD4+ and CD8+ T-cell activation induced by APCs, as shown in Fig. 3.
Tregs also play a key role in maintaining immune homeostasis by inhibiting excessive immune responses. One of the mechanisms through which Tregs suppress effector T-cell activity is via CTLA-4 signaling (19). Two anti-CTLA-4 drugs have been studied in patients with melanoma: i) Ipilimumab, the first ICI evaluated and approved for the treatment of melanoma is a fully human immunoglobulin anti-CTLA-4 monoclonal antibody (20,21); ii) tremelimumab, a fully human immunoglobulin anti-CTLA-4 monoclonal antibody which is still under investigation (12).
There are two major mechanisms through which these drugs act. First, the inhibition of CTLA-4 signaling in cytotoxic T-cells that specifically target tumors can directly affect these cells by enabling them to evade a state of anergy and enter an active proliferative effector phase. Once activated, these effector T-cells are more likely to penetrate the tumor and exhibit direct cytotoxic effects on tumor cells, while also releasing cytokines such as IL-2 and IFN-γ to stimulate an immunogenic tumor microenvironment. Thus, by blocking the CTLA-4 pathway, T-cells that were previously inactive can become activated and effectively target the tumor cells, causing a more powerful immune response against the cancer. This new approach holds promise as a potential immunotherapy for the treatment of cancer (22).
The second major mechanism driving these drugs is the blocking of CTLA-4 signaling in Tregs, which may impair their ability to halt the activity of effector T-cells. This inhibition of CTLA-4 signaling can either cause a decrease in the number of Tregs or reduce their function without affecting their population size. Therefore, blocking CTLA-4 on Tregs may disrupt this suppression and lead to increased immune activation against tumor cells (19,23,24).
Patients with melanoma are treated with the primary aim of suppressing the molecular interplay between the melanoma cells and immune effector cells. Ipilimumab, which has mainly been approved for the treatment of more advanced stages, such as unresectable or metastatic melanoma, has been shown to be associated with a marked overall survival rate confirmed from a phase 3 clinical trial (25). The interference of ipilimumab on CTLA-4 expressed on the subset of tumor-specific T-cell proliferation and B7 molecules on antigen-presenting cells is expected to prevent tumor development (26).
PD-1 pathway and anti-PD-1/PD-L1 drugs
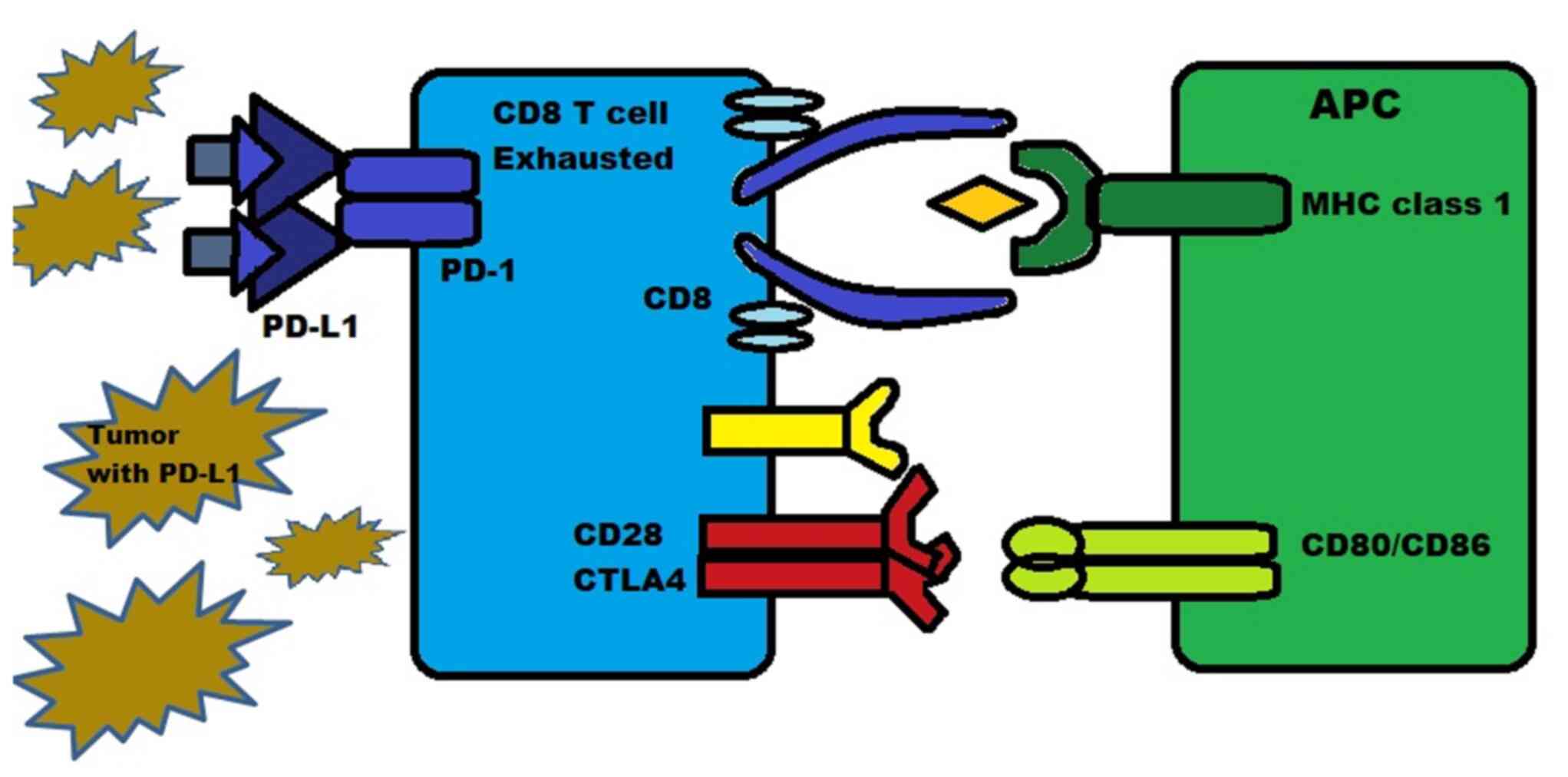
PD-1 is a protein present on the surface of T-cells, B-cells and natural killer (NK) cells. It functions as an inhibitory molecule by binding to PD-L1 (or B7-H1) and PD-L2 (B7-H2). PD-L1 is expressed in numerous types of tissue, including hematopoietic cells and certain tumors such as melanoma, where they are expressed in 40-50% of cases. PD-L2 is mainly expressed in hematopoietic cells. The binding of PD-1 to PD-L1/2 inhibits the death of tumor cells and promotes the conversion of T-effector cells into Tregs, while also inducing exhaustion in peripheral T-effector cells, as illustrated in Fig. 4 (27,28).
PD-1 and/or PD-L1 are also expressed on cells, such as NK cells, monocytes and dendritic cells (27,28). The PD-1 pathway operates through various mechanisms, such as reducing the activity of T-cells during an inflammatory response, increasing the proliferation and suppressive activity of Tregs, and reducing the lytic activity of B-cells and NK cells (29).
The affinity between PD-1 and PD-L1 is 3-fold stronger than the affinity between PD-1 and PD-L2. When PD-L1 binds with PD-1 on T-cells, it results in T-cell exhaustion, dysfunction, neutralization and the production of IL-10 within the tumor mass. This process allows tumors that overexpress PD-L1 to protect themselves from being attacked and killed by CD8+ cytotoxic T-cells (30).
Pro-effector cytokines, namely IL-12 and IFN-γ, can upregulate the expression of PD-1 and PD-L1/L2, which helps to prevent excessive T-effector cell activity. It is worth noting that PD-L1 has also been shown to inhibit CD80, indicating the existence of complex interactions between CTLA-4, PD-1 and other pathways (31,32).
The PD-1 and PD-L1 antibody inhibitors were created with the aim of preventing the PD-1 or PD-L1 side from functioning, reactivating T-cells and promoting an immune response against cancer cells (13).
Based on promising results from clinical trials, antibodies that inhibit PD-1 (such as pembrolizumab, nivolumab-IgG4 fully humanized and dostarlimab), as well as those that inhibit PD-L1 (such as avelumab, atezolizumab, and durvalumab) are being evaluated for use in melanoma cases and various other malignancies (NCT04020809, NCT04274816, NCT03313206, NCT03842943 and NCT05928962). However, it is not yet known which inhibitor, PD-1 or PD-L1, is more efficient (13). Of these, nivolumab and pembrolizumab are the two major FDA-approved anti-PD-1 monoclonal antibodies available for the treatment of advanced and metastatic melanomas.
Melanoma cells exhibit increased levels of PD-L1, which promotes the apoptosis of the likewise increased levels of T-cells (33). It has also been found that the circulating melanoma antigen-specific T-cells and tumor-infiltrating lymphocytes express PD-1 abnormally. It is considered that melanoma cells are capable of initiating, as well as sustaining PD-1 signals, T-cell fatigue and dysfunction (33). Hence, by blocking PD-1 in patients with melanoma, one could possibly restore abnormal activation and signaling and eventually recover the immune effect. Pembrolizumab or lambrolizumab were used in unresectable or metastatic melanoma in the study by Hamid et al (34), in an aim to elucidate the effects of PD-1 medications in melanoma.
However, due to the heterogeneous nature of tumors, the expression of PD-L1 is not uniform throughout. The extent of PD-L1 expression can differ in various locations within the tumor, resulting in varying levels of PD-L1 in immunohistochemical staining. Moreover, the effectiveness of PD-L1/PD-1 inhibitors can also be influenced by several other factors, such as the type of cancer, the patient's immune system and the genetic profile of the tumor. Thus, a more in-depth understanding of these factors is essential for developing effective treatment strategies that consider the heterogeneity of tumors and the variability in PD-L1 expression (35).
The combination ICI therapy used in the treatment of patients with metastatic melanoma primarily involves CTLA-1 and PD-1 inhibitors. This amplified the inhibitions that can be simultaneously intervened during different phases of the interaction among melanoma cells and the immune system. This, for example, includes anti-CTLA-4 inhibiting the priming stage at the same time anti-PD-1 inhibits the effector stage (36,37). It has also been noted that the use of anti-CTLA-4 inhibitors results in an increased expression of PD-1; hence, using combination therapy results in a more robust treatment response in patients with melanoma (38).
Newer drugs
An increased understanding of immunological mechanisms has led to the identification of additional potential targets for checkpoint inhibition in the treatment of cancer. Some of these potential targets include BTLA, VISTA, TIM-3, CD47 and LAG-3. i) The blockade of BTLA has been shown to enhance New York esophageal squamous cell carcinoma 1) specific CD8+ T-cell function and enhance the efficacy of anti-PD-1 (39-41). ii) VISTA blockade has been shown to increase T-cell infiltration and function in tumors, thereby reducing tumor growth (10,42). iii) TIM-3 blockade causes T-helper-1 cell hyperproliferation and cytokine release, leading to tumor shrinkage in a mouse model when combined with anti-CTLA-4 or anti-PD-1 (43-47). iv) Targeting CD47 with a humanized anti-CD47 monoclonal antibody in combination with rituximab has shown to lead to objective responses in half of the heavily pretreated patients with relapsed or refractory non-Hodgkin's lymphoma, including a complete response in more than one-third of patients (48). v) An immune pathway known as LAG-3 has been identified as a potential complement to the PD-1/PDL1 pathway in enhancing the immune response against cancer. LAG-3 is an immune checkpoint receptor that regulates the function of T-cells. BMS-986016 is a therapy that targets LAG-3 and is currently under investigation in combination with nivolumab, which targets PD-1, to enhance the immune response against cancer cells. The combination of these two therapies has the potential to create a synergistic effect, leading to improved treatment outcomes for patients with cancer (49).
4. Combination therapy with immune checkpoint inhibitors in melanoma
The ability of anti-CTLA-4 and anti-PD-1/PD-L1 monoclonal antibodies to target various T-cell activation locations and phases is the rationale for their combined use. PD-1 is primarily expressed on antigen-experienced T-cells in peripheral tissues, while CTLA-4 is expressed by naive T-cells in the lymph nodes. According to pre-clinical research, combining ICIs is more effective than treatment with with monotherapy for managing melanoma (50-53).
In pre-clinical investigations, anti-CTLA-4 and anti-PD-1/PD-L1 monoclonal antibodies have been shown to induce the infiltration of CD8+ T-cells and the expansion of an inducible T-cell co-stimulator (ICOS)+ T helper 1-like CD4 fraction, which in turn induces the response of CD4+ effector T-cells. Based on this, the sequencing or combination of nivolumab with ipilimumab in metastatic cutaneous melanoma has been researched (50-53). Other combination studies are on nivolumab, relatlimab and combination therapy with pembrolizumab with low-dose ipilimumab (54,55). The data from the CheckMate and RELATIVITIY047 trials on the combination of ICIs are presented in Table I, which demonstrate a favorable response for such therapies (54,56,57). Table II presents data from a meta-analysis, comparing monotherapy and combination therapy (47-64).
Table ISummary of the results of the CheckMate and RELATIVITY047 trials performed on the combination of immune checkpoint inhibitors for the treatment of melanoma. |
Table IISummary of results obtained from a previous meta-analysis of clinical trials conducted by Pradeep et al (58), which compared the efficacy and safety of ICIs between monotherapy and combined ICI therapy in advanced melanomas. |
5. Comparison between the immune checkpoint inhibitors
Along with the major breakthrough in melanoma treatment with the use of selective BRAF inhibitors, after ~6 months of the median duration, resistance to therapy began to develop. The BRAF mutation drives the tumor proliferation exponentially by activating mitogen-activated kinase pathway (MAP), and the development of resistance to BRAF inhibitors in both MAP kinase-dependent and MAP kinase-independent pathways (65-67). Resistance in MAP kinase-dependent pathways includes secondary mutations in NRAS, the increased expression of COT kinase, CRAF activation and acquired mutations in MEK1 (65,68-71). MAP kinase-independent pathways include the upregulation of platelet-derived growth factor receptor, additional receptor tyrosine kinases activation including AXL, Erb-B2 receptor tyrosine kinase 4) and insulin like growth factor 1 receptor, the activation of PI3K/AKT signaling, and the loss of phosphatase and tensin homolog (PTEN) (65,69,71-75).
Ipilimumab
Ipilimumab is a fully human monoclonal antibody developed to antagonize CTLA-4. A clinical study was conducted on patients who had unresectable stage III or IV melanoma, where they were randomly assigned in a 3:1:1 ratio to receive ipilimumab (3 mg/kg) plus the glycoprotein 100 (gp100) vaccine, ipilimumab alone, or gp100 alone. The patients who received ipilimumab plus gp100 had a longer median overall survival rate of 10 months compared to 6.4 months for those who received gp100 alone, with a hazard ratio (HR) for mortality of 0.68 and a statistically significant P-value of <0.001. The median overall survival rate of patients who received ipilimumab alone was 10.1 months (HR, 0.66; P=0.003) compared to those who received gp100 alone (20).
In the study by Robert et al (25), patients with untreated metastatic melanoma were randomly assigned to receive either ipilimumab plus dacarbazine or dacarbazine alone. A significantly longer median overall survival (11.2 months) was found in the ipilimumab plus dacarbazine group compared to the dacarbazine alone group (9.1 months). In a follow-up maintenance study, patients who received ipilimumab plus dacarbazine had a higher 5-year survival rate (18.2%) compared to those who received dacarbazine alone (8.8%). These findings suggest that ipilimumab in combination with dacarbazine may be an effective treatment option for metastatic melanoma patients (76).
In a trial for ipilimumab as an adjuvant treatment performed by Eggermont et al (77), patients with stage III cutaneous melanoma who had undergone complete resection were randomly administered either ipilimumab (10 mg/kg) (n=475) or a placebo (n=476). Following a median follow-up of 5.3 years, the ipilimumab group had a 5-year recurrence-free survival rate of 40.8%, while the placebo group had a rate of 30.3% (HR, 0.76; P<0.001). In terms of the 5-year overall survival rate, the ipilimumab group had a rate of 65.4% compared to 54.4% in the placebo group (HR, 0.72; P=0.001) (77).
In the study by Ascierto et al (78), patients with unresectable stage III or IV melanoma were randomly assigned to receive either 10 or 3 mg/kg ipilimumab. The median overall survival rate was 15.7 months for the 10 mg/kg group and 11.5 months for the 3 mg/kg group (HR, 0.84; P=0.04). Overall, their study suggested that ipilimumab treatment improved the survival outcomes of patients with unresectable stage III or IV melanomas, with higher doses of the drug (10 mg/kg) leading to an improved overall survvial compared to lower doses (3 mg/kg) (78).
Nivolumab
Nivolumab is a monoclonal antibody that inhibits the interaction of PD-1 with PD-L1. The clinical study performed by Robert et al (79) compared the efficacy of nivolumab with the standard therapy of dacarbazine. In their study, patients who had metastatic melanoma without a BRAF mutation were randomly divided into two groups (1:1 with nivolumab at 3 mg/kg once every 2 weeks (n=210) and dacarbazine (n=208). The survival rate at 1 year was 72.9% in patients treated with nivolumab compared to 42.1% in patients who were assigned dacarbazine (HR, 0.42, P<0.001). The objective response rate was 40% with nivolumab compared to 13.9% with dacarbazine (odds ratio, 4.06; P<0.001) (79). Another randomized controlled trial was carried out between 2012-2014 on patients with advanced melanoma who progressed after ipilimumab therapy or a combination of ipilimumab and a BRAF inhibitor if they were found to be positive for a V600E mutation (80). That study assessed the role of nivolumab as a second-line treatment in the management of patients with advanced melanoma. Patients were divided into three groups in a 2:1 pattern where one group (n=272) received nivolumab at 3 mg/kg once every 2 weeks and another group (n=133) received the investigator's choice of chemotherapy (ICC), which was either dacarbazine or paclitaxel plus carboplatin (80). An interim analysis of that study found that, in the first 120 patients of the nivolumab group, 38 patients (31.7%) experienced confirmed objective responses, whereas only 5 out of the 47 patients (10.8%) receiving the ICC treatment exhibited similar responses. Subsequently, upon further analysis of that trial, it was revealed that the median overall survival rate of patients who received nivolumab was 16 months, while for those who received ICC, it was 14 months (81). The HR was 0.95, indicating that nivolumab did not improve the survival rate of patients who had ipilimumab-refractory metastatic melanoma when compared to ICC. However, nivolumab had a higher overall response rate of 27% vs. 10% for ICC, and the median duration of response was also longer for nivolumab at 32 months compared to 13 months for ICC (77). Hence, nivolumab exhibiting a higher overall response rate and a longer duration of response suggests that it may be a more effective treatment option for some patients (81). Another study was also carried out to compare the efficacy of nivolumab compared to ipilimumab as an adjuvant therapy in patients who had resected advanced melanoma. In patients with stage III or stage IV melanoma, adjuvant therapy was administered with either nivolumab (n=453) or ipilimumab (n=453) and follow-up was performed after 18 months (82). The 12-month rate of recurrence-free survival was significantly higher in the nivolumab group at 70.5%, vs. 60.8% in the ipilimumab group with a HR of 0.65 (P<0.001). It was also noted that treatment-related adverse events were 14.4% for patients treated with nivolumab and 45.9% for those treated with ipilimumab. Therefore, patients who received ipilimumab therapy experienced more severe side-effects than those who received nivolumab therapy. This suggests that nivolumab may be a more effective and tolerable treatment option for patients with stage IIIB, IIIC, or IV melanoma following surgical resection (82).
Pembrolizumab
Pembrolizumab is a monoclonal antibody which functions by blocking the PD-1 on T-cells and allowing these T-cells to identify and kill cancer cells. Similar to nivolumab, pembrolizumab was also compared with ICC in ipilimumab-refractory melanoma. A randomized controlled study was conducted on patients with advanced melanoma and have progressed even after receiving ipilimumab and/or standard BRAF therapy (83). Patients were divided into three groups as follows: One group (n=181) received 10 mg/kg pembrolizumab, one group (n=180) received 2 mg/kg pembrolizumab, and another group (n=179) received ICC. The 6-month progression-free survival rate was found to be 38% in patients treated with pembrolizumab at 10 mg/kg (HR, 0.5 vs. ICC; P<0.0001), 34% in the 2 mg/kg group (HR, 0.57 vs. ICC; P<0.0001) and 16% in the ICC group (83). Another study was conducted by Robert et al (84), this time comparing pembrolizumab with ipilimumab. Patients with advanced melanoma were divided at a 1:1:1 ratio to receive pembrolizumab at 10 mg/kg once every 2 weeks or pembrolizumab at 2 mg/kg once every 3 weeks or four doses of ipilimumab at 3 mg/kg for once every 3 weeks. An interim analysis was performed which revealed that the 6-month progression-free survival of the patients treated with pembrolizumab once every 2 weeks was 47.3% (HR, 0.58 vs. ipilimumab; P<0.001), 46.4% for those treated with pembrolizumab once every 3 weeks (HR, 0.58 vs. ipilimumab; P<0.001) and 26.5% for those treated with ipilimumab (84). A final analysis revealed that the median overall survival rate was not reached in both pembrolizumab groups; however, it was noted to be 16 months in the ipilimumab group (HR, 0.68 for pembrolizumab once every 2 weeks vs. ipilimumab, P=0.0009; and HR, 0.68 for pembrolizumab once every 3 weeks vs. ipilimumab, P=0.0008) (85). Similarly, in the study by Robert et al (84) the 24-month overall survival rate was 55% in the group treated once every 2 weeks, 55% in the group treated once every 3 weeks and 43% in the ipilimumab group. Not only do nivolumab and pembrolizumab prolong overall survival, but they also maintain the quality of life of patients with melanoma (86,87). These findings have led to the FDA approval of pembrolizumab for ipilimumab and/or BRAF inhibitory refractory advanced melanoma. A summary of the comparison among ICIs and their outcomes in patients is presented in Table III.
Table IIIIndividual immune checkpoint inhibitors with the various outcomes affecting clinical decisions regarding their use. |
6. Biomarkers
The prognostic marker for melanoma traditionally used is the depth of invasion and the associated mitotic count of the affected cells. With advancements being made, newer prognostic markers have been found and used. Prognostic and predictive biomarkers have gained importance, particularly in the treatment of melanoma.
Serum biomarkers
The role of serum biomarkers in the early detection of melanoma is described in Table IV (88-106).
Tissue markers. Prognostic markers
i) Tumor infiltrating lymphocyte (TIL) patterns are often divided into grades, such as ‘absent’, which is no presence of any lymphocytes within the tumor, ‘non-brisk’, which suggest few foci of lymphocytes within the tumor, or ‘brisk’, which is a large diffuse infiltration of lymphocytes within the tumor (107). As demonstrated by Clark et al (107) in 1989, as well as by others, the presence of brisk TILs in a vertical growth pattern is often associated with a favorable disease-specific survival and overall survival rate after non-brisk and absent patterns of TILs (107,108).
ii) Histotype: The majority of melanoma histotypes are not considered prognostic when looked at individually from tumor thickness, and are therefore not included in the American Joint Committee on Cancer staging system (90,109,110). However, a nodular melanoma is an independent predictor which can be used for the measurement of recurrence and its association with mortality due to melanoma (111).
iii) Digital images trained from AI: New advancements have allowed for the development of deep learning-based biomarkers, which can help to stratify the stages of melanoma into risk groups, and thus associate disease-specific survival with two independent validating cohorts to accurately predict the prognosis of patients with early-stage melanoma (112).
iv) Melanoma cell adhesion molecule (MCAM): Expressed in 80% of metastatic tumors, MCAM is a cell adhesion marker (113). Those who are positive for MCAM have significantly worse 5-year survival rates than those who are negative for MCAM, and there is an inverse association between the amount of marker expressed and survival (114,115).
v) Ki-67: Ki-67 is a unique nuclear antigen that can function as a marker for cellular proliferation during the active phase of the cell cycle (116). For melanomas who have a thickness <1 mm, the risk of metastasis increases with the expression of Ki-67 and an increased mitotic rate (117). However, with the increasing thickness of melanomas, Ki-67 can serve as a more effective prognostic marker than the mitotic rate, and is often associated with ulceration within the tumor, necrosis, higher level Clark's level of invasion, and even vascular invasion (118). In addition, with recurrent melanomas, higher values of Ki-67 exhibit an independent association with a decreased overall survival (119).
vi) Lymphatic invasion: In research on primary melanomas with a thickness >1 mm, D2-40 staining was assessed for lymphatic invasion, which is an antibody against sialoglycoprotein that selectively attaches on endothelial cells of lymphatic vessels and helps detect sentinel lymph node metastasis (120-122).
vii) Osteopontin: Overexpressed in numerous visceral malignancies, osteopontin is known as an integrin-binding protein and used as a biomarker to measure tumor progress and metastasis (123-125). It functions as an independent predictor for the prognosis of melanoma and was found to be associated with increased sentinel lymph node positivity in a cohort of 345 patients who had primary melanoma detected using immunohistochemical analysis (126).
viii) Driver mutations: It has been found that BRAF and NRAS are associated with a significantly lower melanoma-specific survival in high-risk tumors, such as a stage >2(127). NF1 mutations has also been found to be associated with a lower disease-specific survival and overall survival (128). However, further research is required to identify patients with BRAF mutations and uncover the role of BRAF mutations in directing the treatment strategy.
Predictive markers. The role of predictive markers in melanoma and its clinical importance is summarized in Table V (61,129-151).
7. Factors affecting drug use
Therapy with nivolumab affects the frequencies of innate lymphoid cells (ILCs) in peripheral blood in patients with melanoma. The frequency, as well as the secretory activity of ILC subsets, particularly ILC2s, are affected by treatment. Albeit nivolumab was found to not effectively alter serum cytokine profiles, pro-inflammatory and angiogenic substances such as IL-1, IL-6, CCL2, CXCL8 and VEGF had levels outside the normal range in 7 of the 18 cytokines. In addition, the production of IL-5 and IL-13 was affected, which are released during parasite infections and allergic reactions (152). In malignant melanoma, type 3 ILC is suspected in tumor suppression (153). Serum levels of IL-6, CXCL8 and CCL2 in particular, surge during melanoma progression, while mature NKp44+ ILC3s protect against melanoma (154).
As previously demonstrated, the advancement of melanoma was comparable with aging, although the treatment outcome did not differ significantly, and there was no significant change in the survival outcomes of elderly patients as compared to young ones. Moreover, it was recommended that both age groups should be treated in similar manner (155). Primary and secondary resistance are also a key factor affecting drug use (84,156). Combination therapy with ipilimumab and nivolumab, as approved by the FDA, has been proven to be efficient (157). There is an increased incidence of melanoma among women of reproductive age. As opposed to this, postmenopausal women have a relatively low incidence of the disease, thus raising the possibility that sex hormones such as estrogen may be involved in the growth of the disease (158). As a result, estrogen levels should be considered an important biomarker in advanced melanoma. Elderly patients aged ≥65 treated with combination therapy comprising of ipilimumab and nivolumab have not exhibited a considerable difference in overall mortality. When prior exposure to ipilimumab is considered, women have a 2.82-fold increased risk of mortality as compared to prior-exposed males with ipilimumab (158).
Moderate colitis which does not require the use of intravenous steroids is consistent with an improved overall survival of patients with stage IV melanoma when treated with a single anti-CTLA-4 drug, but not with combination drugs. This holds true even after the completion of therapy (159). Multiple nonrandomized studies have shown excellent results in patients who discontinue treatment after being treated for 1-2 years and disease progression is also uncommon in the following 2-5 years of treatment termination (160-162). This is in contrast to the progression of disease of patients with non-small cell lung cancer, for whom treatment continuation led to improved results compared to treatment termination (163).
8. Adverse effects
The use of PD-1 inhibitors, namely nivolumab and pembrolizumab, and the anti-CTLA-4 drug, ipilimumab, has been shown to be associated with a steady regression in malignancies, including metastatic melanoma (164).
PD-1 inhibitors function in the tumor setting, while CTLA-4 inhibitors act on lymphoid tissue, resulting in a wide and different set of adverse events (165). Combination therapies with nivolumab and ipilimumab have been proven to be more effective with a response rate of 59% as compared to when used alone, with response rate of 43% for nivolumab and 15-20% for ipilimumab. Moreover, an increased response rate is associated with an increase in adverse events, resulting in an overall increase in adverse events with the combination of nivolumab with ipilimumab, as compared to nivolumab or ipilimumab monotherapy (36,62).
A CTLA-4 blockade with or without anti-PD-1 antibody produces adverse events in a dose-dependent manner (166,167). Considering that older patients are more inclined to develop rheumatologic events and female patients are also at an increased risk, the toxicity profile may vary according to age and sex (168,169).
However, as these molecules are targeted, due to the resulting immune response, an increase in the incidence of autoimmune conditions is observed; these adverse events are known as immune-related adverse events (irAE). If severe irAEs occur with one of the drugs, then it is a safe practice to re-challenge the patient with a different class of drug (165). These drugs have the following on the following systems.
Gastrointestinal tract
Diarrhea is the most frequent irAE with incidences between 10 and 13% (164).
Endocrine disorders
In decreasing order, the first endocrine system that is most affected by ICIs is the thyroid gland (typically hypothyroidism observed following a transient thyroiditis-induced thyrotoxicosis) followed by the rest of the endocrine organs. The median time frame from the start of the treatment to the development of thyroid symptoms, most commonly hypothyroidism, is 6 weeks, followed by pituitary (hypophysitis), adrenals (primary adrenal insufficiency) and β-cells of the pancreas (insulin deficient diabetes, analogous to type 1 diabetes) (170). These are different from the side-effects brought on by conventional cytotoxic chemotherapy or even more recent molecular-targeted medicines, which infrequently result in endocrine dysfunction (171).
Skin disorders
Non-specific adverse events such as maculopapular rash, pruritus, psoriasiform, eczematous and lichenoid dermatosis are among the most prevalent (172,173). Compared to anti-PD-1 monotherapy, the maculopapular rash phenotype is more prevalent when CTLA-4 inhibition is implemented (21). Bullous pemphigoid, vitiligo-like skin hypopigmentation/depigmentation and alopecia are other less-common irCAEs (174,175). Although severe reactions, such as Stevens-Johnson syndrome, toxic epidermal necrolysis and drug reaction with eosinophilia and systemic symptoms are uncommon, cutaneous consequences are typically self-limiting (174-176). Early diagnosis and the administration of corticosteroids or antitumor necrosis factor-agents are the foundation of treatment algorithms for irCAEs (176,177). However, the use of corticosteroids before or after ICI initiation may result in a diminished antitumor efficacy. Anti-CTLA-4 and anti-PD1 therapy have both been associated with reports of vitiligo (178). The occurrence of skin hypopigmentation or depigmentation such as vitiligo has been linked to an extensive anticancer benefit from drug treatment in patients with melanoma. Vitiligo has been proven as a positive predictive factor in measuring the tumor response to treatment. In comparison with the general population, patients with melanoma have a 10-fold increased incidence of drug-related cutaneous hypopigmentation and depigmentation (179). Since the PD-L1:PD1 pathway mostly regulates the peripheral tolerance of melanosomal proteins (such as tyrosinase and TRP-2), the interference of PD-1 signaling may result in autoimmune vitiligo (180). This offers a reasonable explanation for the onset and durability of depigmentation in patients receiving immunotherapy.
Lungs
Case series studies have demonstrated that patients develop organizing pneumonia, diffuse alveolar damage, acute respiratory distress syndrome (ARDS) and non-specific interstitial pneumonia, which is then managed by intravenous and oral steroids (181-185).
Liver and kidneys
A previous meta-analysis revealed adverse effects associated with the use of anti-PD-1/PD-L1 monoclonal antibodies for malignancies with an increased incidence of pancreatitis, and increased levels of liver enzymes, such as aspartate aminotransferase and alanine transaminase, elevated creatinine levels, nephritis and renal failure (164).
9. Mechanisms of resistance
A myriad of ongoing clinical trials and practices have discovered multiple mechanisms leading to resistance to ICIs. More precisely, these include changes in the tumor microenvironment prohibiting T-cell interaction, tumor invasion and tumor cell destruction by effector mechanisms. The key to tumor cell destruction via effector T-cells is through the processing of tumor antigens to antigen-presenting cells. The failure of antigen-presenting components in this pathway is a major cause of resistance in melanoma (186). β2 microglobulin is an key molecule responsible for the folding and transportation of major histocompatibility complex-1 to the surface of cells. Mutations in these molecules have been noted in patients with melanoma at the time of anti-PD1 treatment failure (187). Other mechanisms responsible for limiting T-cell trafficking in the tumor microenvironment include mutations in BRAF, and the inhibition of PTEN. This leads to the increased expression of immunosuppressive molecules, such as VEGF (188). It also inhibits the migration and trafficking of effector T-cells (189). In addition to these tumor-intrinsic mechanisms, various tumor-extrinsic mechanisms also play a role in the development of resistance to ICIs. These include the development of new inhibitory checkpoints, immunosuppressive cytokines and molecules in the tumor microenvironment suppressing immune cell function. One such example is the production of transforming growth factor β (TGF-β) by tumor cells. TGF-β is an immunosuppressive cytokine that functions by stimulating Tregs and inhibiting the cytotoxicity of effector T-cells (190).
To summarize, understanding and investigating the potential mechanisms that lead to resistance to ICIs is crucial in developing effective strategies to guide therapy. Further studies are required to identify new mechanisms and develop targeted therapies to improve the clinical outcome of patients undertaking immunotherapy.
10. Emerging newer therapeutic strategies: Targeting tumor metabolic dependencies
Tumor cells sustain themselves by utilizing altered metabolic pathways by using nutrients, such as glucose, tryptophan and arginine to produce toxic metabolites such as adenosine, lactate and kynurenine (191,192). Such toxic metabolites produce an unfavorable environment for the antitumor cells to function resulting in increased expression of immune checkpoints and expansion of Tregs (193).
The mechanism that tumor cells use is the mutation in the myelocytomatosis oncogene (MYC) and PI3K/AKT/mammalian target of rapamycin (mTOR) signaling pathways. The increased expression of hypoxia-inducible factor-1-α leads to the overexpression of the PI3K/AKT/mTOR pathway, as well as glucose transporters such as glucose transporter 1, leading to increased glucose consumption and acidification of the tumor microenvironment (194,195). As hypoxia is generated, glucose depletion occurs and increased toxic waste is produced within the tumor microenvironment, resulting in the inhibition of tumor antigen presentation by APCs (196). Thus, there is an overall decrease in the antitumor immune response by T-effector, macrophages or NK cells, while pro-tumor immune cells such as Tregs proliferate to increase the expression of inhibitory checkpoint ligand PD-1 on immune cells, inhibiting the antitumor immunity (197). With the advancement of technologies, newer therapeutic strategies that target the immunosuppressive tumor microenvironment generated by tumor cells may be developed to reprogram the behavior of immune cells, leading to an improved efficacy in terms of the treatment response.
One of the important T-cellular processes is the activation of the PI3K pathway, which plays a vital role in proliferation and differentiation. Monotherapy, which inhibits the PI3K pathway, has not yielded any significant results in the treatment of cancer; however, combining PI3K inhibitors and the PD-1-PDL1 blockade has shown some notable results (198). The loss of PTEN, which is a PI3K-inhibiting tumor suppressor often mutated in tumor cells, results in the uncontrolled growth of tumor cells and escapes the immune destruction imposed on it. As previously demonstrated, when mice with PTEN-null melanoma were treated in vivo with the PI3Kβ inhibitor, GSK2636771, this resulted in a decreased AKT phosphorylation and the activation of mTOR targets. Additionally, when it was combined with an anti-PD1 antibody, it markedly improved the survival and increased immune response with reduced tumor cell mass (199). With such promising results, a number of newer anti-PI3K medicines are being developed and tested to increase efficacy (NCT01390818). Despite this, more novel promising approaches are needed to prove the success of combining anti-PI3K drugs with ICIs in the treatment of melanoma (200).
11. Conclusion and future perspectives
The development of ICIs and targeted therapies has played a crucial role in revolutionizing the management of melanomas by improving the overall and progression-free survival. Although both of these therapies have advantages and disadvantages, combination therapy (ICI + ICI, or ICI + targeted therapies) has been found to be more effective in improving patient outcomes. However, there is limited literature available regarding combination therapies and different types of potential combinations. There are also insufficient data on patients and their responses to draw sufficient conclusions. The development of drug-related adverse effects with the use of combination therapies is also a debatable question. However, when developing newer ICIs to achieve a more effective response, a focus should certainly be placed on the integration of nanotechnology or antibody engineering. Through these, one can increase drug delivery to a specific target and thus increase overall response. In addition, focusing on epigenetic modulation and developing ICIs that target those changes can enhance the responsiveness of ICIs.
There may be concerns regarding resistance to ICIs in patients with melanoma. Some patients may have resistance to certain ICIs from the beginning or may develop them as an acquired resistance with subsequent treatment after progression of a tumor with clinical benefit. Further treatment decisions shall be made on the basis of evaluation of the tumor and factors related to the patient, focusing on targeted therapeutic drugs, other immunotherapy drugs, cellular therapies, intralesional therapies, or chemotherapy. It is important to tailor ICI treatment based on an individual's genetic makeup and tumor characteristics to decrease the resistance. The early identification of tumor biomarkers can predict future responses to particular ICIs and may help to select a personalized treatment strategy. Furthermore, with the use of tumor metabolic pathway inhibitors in combination with ICIs, targeting signaling pathways and immune responses can be better used to overcome potential resistance to ICIs than when used alone.
Trials are being conducted on newer inhibitory immune checkpoint targets, as well as certain inhibitory targets beyond immune checkpoints. These include LAF-3, TIM-3, B7-H3 and B7-H4, CD73, etc. which are immune checkpoints, and CEACAM1, CEACAM5/6, CCL2/CCR2, etc. which are other inhibitory targets (201). It is essential to maintain enrollment in clinical trials so that newer ICIs, additional inhibitory treatments, combination therapy, and mechanisms of resistance and methods of overcoming the resistance can all be further investigated.
In conclusion, with the increasing incidence of melanoma over the past two decades, managing it with different treatment modalities has become cumbersome. With the limited effectiveness of the traditional approach using chemotherapy and immunotherapy, the role of newer treatment modalities should be given equal emphasis. Novel approaches using ICIs have been a revolution in the therapeutic approach by unleashing the immune system's ability to recognize and eliminate cancer cells. Ipilimumab, nivolumab and pembrolizumab have been shown to lead to a substantial improvement in the overall survival of patients with advanced melanoma, particularly in high-risk metastatic melanoma compared to traditional therapies. However, with ICIs, it is paramount to monitor any side-effects, and to ensure the optimal outcome is achieved using personalized treatment approaches.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
VS, VP and AS were involved in the conceptualization of the study. VS, VP, AS, BV, SB and SA were involved in the curation of data from the literature for inclusion in the present review. VS, VP and AS were involved in selecting the relevant literature. VS, VP and AS were involved in project administration. VS supervised the study. VS, VP, AS, BV, SB and SA were involved in the writing of the original draft. VS, VP and AS were involved in the writing, review and editing of the manuscript. All authors have read and approved the final manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Finn L, Markovic SN and Joseph RW: Therapy for metastatic melanoma: The past, present, and future. BMC Med. 10(23)2012.PubMed/NCBI View Article : Google Scholar | |
|
Arnold M, Singh D, Laversanne M, Vignat J, Vaccarella S, Meheus F, Cust AE, de Vries E, Whiteman DC and Bray F: Global burden of cutaneous melanoma in 2020 and projections to 2040. JAMA Dermatol. 158:495–503. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Miller AJ and Mihm MC Jr: Melanoma. N Engl J Med. 355:51–65. 2006.PubMed/NCBI View Article : Google Scholar | |
|
Rosenberg SA, Lotze MT, Yang JC, Topalian SL, Chang AE, Schwartzentruber DJ, Aebersold P, Leitman S, Linehan WM, Seipp CA, et al: Prospective randomized trial of high-dose interleukin-2 alone or in conjunction with lymphokine-activated killer cells for the treatment of patients with advanced cancer. J Natl Cancer Inst. 85:622–632. 1993.PubMed/NCBI View Article : Google Scholar | |
|
Bronte V and Mocellin S: Suppressive influences in the immune response to cancer. J Immunother. 32:1–11. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Mellman I, Coukos G and Dranoff G: Cancer immunotherapy comes of age. Nature. 480:480–489. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Pardoll DM: The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 12:252–264. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Okazaki T, Okazaki IM, Wang J, Sugiura D, Nakaki F, Yoshida T, Kato Y, Fagarasan S, Muramatsu M, Eto T, et al: PD-1 and LAG-3 inhibitory co-receptors act synergistically to prevent autoimmunity in mice. J Exp Med. 208:395–407. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Fourcade J, Sun Z, Pagliano O, Chauvin JM, Sander C, Janjic B, Tarhini AA, Tawbi HA, Kirkwood JM, Moschos S, et al: PD-1 and Tim-3 regulate the expansion of tumor antigen-specific CD8+ T cells induced by melanoma vaccines. Cancer Res. 74:1045–1055. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Lines JL, Pantazi E, Mak J, Sempere LF, Wang L, O'Connell S, Ceeraz S, Suriawinata AA, Yan S, Ernstoff MS and Noelle R: VISTA is an immune checkpoint molecule for human T-cells. Cancer Res. 74:1924–1932. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Hanaizi Z, van Zwieten-Boot B, Calvo G, Lopez AS, van Dartel M, Camarero J, Abadie E and Pignatti F: The European medicines agency review of ipilimumab (Yervoy) for the treatment of advanced (unresectable or metastatic) melanoma in adults who have received prior therapy: Summary of the scientific assessment of the committee for medicinal products for human use. Eur J Cancer. 48:237–242. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Tarhini AA: Tremelimumab: A review of development to date in solid tumors. Immunotherapy. 5:215–229. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Wang D, Wang T, Liu J, Yu H, Jiao S, Feng B, Zhou F, Fu Y, Yin Q, Zhang P, et al: Acid-activatable versatile micelleplexes for PD-L1 blockade-enhanced cancer photodynamic immunotherapy. Nano Lett. 16:5503–5513. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Ottaviano M, De Placido S and Ascierto PA: Recent success and limitations of immune checkpoint inhibitors for cancer: A lesson from melanoma. Virchows Arch. 474:421–432. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Chambers CA, Sullivan TJ and Allison JP: Lymphoproliferation in CTLA-4-deficient mice is mediated by costimulation-dependent activation of CD4+ T-cells. Immunity. 7:885–895. 1997.PubMed/NCBI View Article : Google Scholar | |
|
Tivol EA, Borriello F, Schweitzer AN, Lynch WP, Bluestone JA and Sharpe AH: Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 3:541–547. 1995.PubMed/NCBI View Article : Google Scholar | |
|
Waterhouse P, Penninger JM, Timms E, Wakeham A, Shahinian A, Lee KP, Thompson CB, Griesser H and Mak TW: Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science. 270:985–988. 1995.PubMed/NCBI View Article : Google Scholar | |
|
Walker LSK and Sansom DM: The emerging role of CTLA4 as a cell-extrinsic regulator of T cell responses. Nat Rev Immunol. 11:852–863. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Ménard C, Ghiringhelli F, Roux S, Chaput N, Mateus C, Grohmann U, Caillat-Zucman S, Zitvogel L and Robert C: Ctla-4 blockade confers lymphocyte resistance to regulatory T-cells in advanced melanoma: Surrogate marker of efficacy of tremelimumab? Clin Cancer Res. 14:5242–5249. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, et al: Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 363:711–723. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Phan GQ, Yang JC, Sherry RM, Hwu P, Topalian SL, Schwartzentruber DJ, Restifo NP, Haworth LR, Seipp CA, Freezer LJ, et al: Cancer regression and autoimmunity induced by cytotoxic T lymphocyte-associated antigen 4 blockade in patients with metastatic melanoma. Proc Natl Acad Sci USA. 100:8372–8377. 2003.PubMed/NCBI View Article : Google Scholar | |
|
Malek TR and Castro I: Interleukin-2 receptor signaling: At the interface between tolerance and immunity. Immunity. 33:153–165. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Reuben JM, Lee BN, Li C, Gomez-Navarro J, Bozon VA, Parker CA, Hernandez IM, Gutierrez C, Lopez-Berestein G and Camacho LH: Biologic and immunomodulatory events after CTLA-4 blockade with ticilimumab in patients with advanced malignant melanoma. Cancer. 106:2437–2444. 2006.PubMed/NCBI View Article : Google Scholar | |
|
Ribas A, Comin-Anduix B, Economou JS, Donahue TR, de la Rocha P, Morris LF, Jalil J, Dissette VB, Shintaku IP, Glaspy JA, et al: Intratumoral immune cell infiltrates, FoxP3, and indoleamine 2,3-dioxygenase in patients with melanoma undergoing CTLA4 blockade. Clin Cancer Res. 15:390–399. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Robert C, Thomas L, Bondarenko I, O'Day S, Weber J, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, et al: Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 364:2517–2526. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Buchbinder EI and Desai A: CTLA-4 and PD-1 pathways: Similarities, differences, and implications of their inhibition. Am J Clin Oncol. 39:98–106. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Amarnath S, Mangus CW, Wang JCM, Wei F, He A, Kapoor V, Foley JE, Massey PR, Felizardo TC, Riley JL, et al: The PDL1-PD1 axis converts human TH1 cells into regulatory T-cells. Sci Transl Med. 3(111ra120)2011.PubMed/NCBI View Article : Google Scholar | |
|
Spranger S, Spaapen RM, Zha Y, Williams J, Meng Y, Ha TT and Gajewski TF: Up-regulation of PD-L1, IDO, and T(regs) in the melanoma tumor microenvironment is driven by CD8(+) T cells. Sci Transl Med. 5(200ra116)2013.PubMed/NCBI View Article : Google Scholar | |
|
Sun Z, Fourcade J, Pagliano O, Chauvin JM, Sander C, Kirkwood JM and Zarour HM: IL10 and PD-1 cooperate to limit the activity of tumor-specific CD8+ T cells. Cancer Res. 75:1635–1644. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Zou W and Chen L: Inhibitory B7-family molecules in the tumour microenvironment. Nat Rev Immunol. 8:467–477. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Kinter AL, Godbout EJ, McNally JP, Sereti I, Roby GA, O'Shea MA and Fauci AS: The common gamma-chain cytokines IL-2, IL-7, IL-15, and IL-21 induce the expression of programmed death-1 and its ligands. J Immunol. 181:6738–6746. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Yang J, Riella LV, Chock S, Liu T, Zhao X, Yuan X, Paterson AM, Watanabe T, Vanguri V, Yagita H, et al: The novel costimulatory programmed death ligand 1/B7.1 pathway is functional in inhibiting alloimmune responses in vivo. J Immunol. 187:1113–1119. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Krönig H, Julia Falchner K, Odendahl M, Brackertz B, Conrad H, Muck D, Hein R, Blank C, Peschel C, Haller B, et al: PD-1 expression on Melan-A-reactive T cells increases during progression to metastatic disease. Int J Cancer. 130:2327–2336. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, et al: Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 369:134–144. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, Kuchroo VK and Sharpe AH: PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med. 206:3015–3029. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M, Rutkowski P, et al: Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 373:23–34. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, Lao CD, Wagstaff J, Schadendorf D, Ferrucci PF, et al: Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 377:1345–1356. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Marconcini R, Spagnolo F, Stucci LS, Ribero S, Marra E, Rosa F, Picasso V, Di Guardo L, Cimminiello C, Cavalieri S, et al: Current status and perspectives in immunotherapy for metastatic melanoma. Oncotarget. 9:12452–12470. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Watanabe N, Gavrieli M, Sedy JR, Yang J, Fallarino F, Loftin SK, Hurchla MA, Zimmerman N, Sim J, Zang X, et al: BTLA is a lymphocyte inhibitory receptor with similarities to CTLA-4 and PD-1. Nat Immunol. 4:670–679. 2003.PubMed/NCBI View Article : Google Scholar | |
|
Murphy KM, Nelson CA and Sedý JR: Balancing co-stimulation and inhibition with BTLA and HVEM. Nat Rev Immunol. 6:671–681. 2006.PubMed/NCBI View Article : Google Scholar | |
|
Fourcade J, Sun Z, Pagliano O, Guillaume P, Luescher IF, Sander C, Kirkwood JM, Olive D, Kuchroo V and Zarour HM: CD8(+) T cells specific for tumor antigens can be rendered dysfunctional by the tumor microenvironment through upregulation of the inhibitory receptors BTLA and PD-1. Cancer Res. 72:887–896. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Le Mercier I, Chen W, Lines JL, Day M, Li J, Sergent P, Noelle RJ and Wang L: VISTA regulates the development of protective antitumor immunity. Cancer Res. 74:1933–1944. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T, Manning S, Greenfield EA, Coyle AJ, Sobel RA, et al: Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature. 415:536–541. 2002.PubMed/NCBI View Article : Google Scholar | |
|
Anderson AC, Anderson DE, Bregoli L, Hastings WD, Kassam N, Lei C, Chandwaskar R, Karman J, Su EW, Hirashima M, et al: Promotion of tissue inflammation by the immune receptor Tim-3 expressed on innate immune cells. Science. 318:1141–1143. 2007.PubMed/NCBI View Article : Google Scholar | |
|
Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ, Zheng XX, Strom TB and Kuchroo VK: The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity. Nat Immunol. 6:1245–1252. 2005.PubMed/NCBI View Article : Google Scholar | |
|
Sabatos CA, Chakravarti S, Cha E, Schubart A, Sánchez-Fueyo A, Zheng XX, Coyle AJ, Strom TB, Freeman GJ and Kuchroo VK: Interaction of Tim-3 and Tim-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat Immunol. 4:1102–1110. 2003.PubMed/NCBI View Article : Google Scholar | |
|
Ngiow SF, von Scheidt B, Akiba H, Yagita H, Teng MWL and Smyth MJ: Anti-TIM3 antibody promotes T cell IFN-γ-mediated antitumor immunity and suppresses established tumors. Cancer Res. 71:3540–3551. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Advani R, Flinn I, Popplewell L, Forero A, Bartlett NL, Ghosh N, Kline J, Roschewski M, LaCasce A, Collins GP, et al: CD47 blockade by Hu5F9-G4 and rituximab in non-Hodgkin's lymphoma. N Engl J Med. 379:1711–1721. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Ascierto PA, Melero I, Bhatia S, Bono P, Sanborn RE, Lipson EJ, Callahan MK, Gajewski T, Gomez-Roca CA, Hodi FS, et al: Initial efficacy of anti-lymphocyte activation gene-3 (anti-LAG-3; BMS-986016) in combination with nivolumab (nivo) in pts with melanoma (MEL) previously treated with anti-PD-1/PD-L1 therapy. J Clin Orthod. 35 (15 Suppl)(S9520)2017. | |
|
Wei SC, Levine JH, Cogdill AP, Zhao Y, Anang NAS, Andrews MC, Sharma P, Wang J, Wargo JA, Pe'er D and Allison JP: Distinct cellular mechanisms underlie anti-CTLA-4 and anti-PD-1 checkpoint blockade. Cell. 170:1120–1133.e17. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Rotte A, Jin JY and Lemaire V: Mechanistic overview of immune checkpoints to support the rational design of their combinations in cancer immunotherapy. Ann Oncol. 29:71–83. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Tarhini A: Immune-mediated adverse events associated with ipilimumab ctla-4 blockade therapy: The underlying mechanisms and clinical management. Scientifica (Cairo). 2013(857519)2013.PubMed/NCBI View Article : Google Scholar | |
|
Michot JM, Bigenwald C, Champiat S, Collins M, Carbonnel F, Postel-Vinay S, Berdelou A, Varga A, Bahleda R, Hollebecque A, et al: Immune-related adverse events with immune checkpoint blockade: A comprehensive review. Eur J Cancer. 54:139–148. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Tawbi HA, Schadendorf D, Lipson EJ, Ascierto PA, Matamala L, Castillo Gutiérrez E, Rutkowski P, Gogas HJ, Lao CD, De Menezes JJ, et al: Relatlimab and nivolumab versus nivolumab in untreated advanced melanoma. N Engl J Med. 386:24–34. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Olson DJ, Eroglu Z, Brockstein B, Poklepovic AS, Bajaj M, Babu S, Hallmeyer S, Velasco M, Lutzky J, Higgs E, et al: Pembrolizumab plus ipilimumab following anti-PD-1/L1 failure in melanoma. J Clin Oncol. 39:2647–2655. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Weber JS, Gibney G, Sullivan RJ, Sosman JA, Slingluff CL Jr, Lawrence DP, Logan TF, Schuchter LM, Nair S, Fecher L, et al: Sequential administration of nivolumab and ipilimumab with a planned switch in patients with advanced melanoma (CheckMate 064): An open-label, randomised, phase 2 trial. Lancet Oncol. 17:943–955. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Shoushtari AN, Wagstaff J, Ascierto PA, Butler MO, Lao CD, Marquez-Rodas I, Chiarion-Sileni V, Dummer R, Ferrucci PF, Lorigan P, et al: CheckMate 067: Long-term outcomes in patients with mucosal melanoma. J Clin Orthod. 38 (15 Suppl)(S10019)2020. | |
|
Pradeep J, Win TT, Aye SN and Sreeramareddy CT: Efficacy and safety of immune checkpoint inhibitors for advanced malignant melanoma: A meta-analysis on monotherapy vs combination therapy. J Cancer. 13:3091–3102. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Amaria RN, Reddy SM, Tawbi HA, Davies MA, Ross MI, Glitza IC, Cormier JN, Lewis C, Hwu WJ, Hanna E, et al: Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat Med. 24:1649–1654. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Hodi FS, Chesney J, Pavlick AC, Robert C, Grossmann KF, McDermott DF, Linette GP, Meyer N, Giguere JK, Agarwala SS, et al: Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-Year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 17:1558–1568. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Hodi FS, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Cowey CL, Lao CD, Schadendorf D, Wagstaff J, Dummer R, et al: Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-Year outcomes of a multicentre, randomised, phase 3 trial. Lancet Oncol. 19:1480–1492. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Lao CD, Cowey CL, Schadendorf D, Wagstaff J, Dummer R, et al: Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 381:1535–1546. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Postow MA, Chesney J, Pavlick AC, Robert C, Grossmann K, McDermott D, Linette GP, Meyer N, Giguere JK, Agarwala SS, et al: Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 372:2006–2017. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Long GV, Atkinson V, Lo S, Sandhu S, Guminski AD, Brown MP, Wilmott JS, Edwards J, Gonzalez M, Scolyer RA, et al: Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: A multicentre randomised phase 2 study. Lancet Oncol. 19:672–681. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Wagle N, Emery C, Berger MF, Davis MJ, Sawyer A, Pochanard P, Kehoe SM, Johannessen CM, Macconaill LE, Hahn WC, et al: Dissecting therapeutic resistance to RAF inhibition in melanoma by tumor genomic profiling. J Clin Oncol. 29:3085–3096. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN and Sawyers CL: Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science. 293:876–880. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Ellis LM and Hicklin DJ: Resistance to targeted therapies: Refining anticancer therapy in the era of molecular oncology. Clin Cancer Res. 15:7471–7478. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, Chen Z, Lee MK, Attar N, Sazegar H, et al: Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 468:973–977. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Johannessen CM, Boehm JS, Kim SY, Thomas SR, Wardwell L, Johnson LA, Emery CM, Stransky N, Cogdill AP, Barretina J, et al: COT drives resistance to RAF inhibition through MAP kinase pathway reactivation. Nature. 468:968–972. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Montagut C, Sharma SV, Shioda T, McDermott U, Ulman M, Ulkus LE, Dias-Santagata D, Stubbs H, Lee DY, Singh A, et al: Elevated CRAF as a potential mechanism of acquired resistance to BRAF inhibition in melanoma. Cancer Res. 68:4853–4861. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Villanueva J, Vultur A, Lee JT, Somasundaram R, Fukunaga-Kalabis M, Cipolla AK, Wubbenhorst B, Xu X, Gimotty PA, Kee D, et al: Acquired resistance to BRAF inhibitors mediated by a RAF kinase switch in melanoma can be overcome by cotargeting MEK and IGF-1R/PI3K. Cancer Cell. 18:683–695. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Turke AB, Zejnullahu K, Wu YL, Song Y, Dias-Santagata D, Lifshits E, Toschi L, Rogers A, Mok T, Sequist L, et al: Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell. 17:77–88. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, Lindeman N, Gale CM, Zhao X, Christensen J, et al: MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 316:1039–1043. 2007.PubMed/NCBI View Article : Google Scholar | |
|
Guix M, Faber AC, Wang SE, Olivares MG, Song Y, Qu S, Rinehart C, Seidel B, Yee D, Arteaga CL and Engelman JA: Acquired resistance to EGFR tyrosine kinase inhibitors in cancer cells is mediated by loss of IGF-binding proteins. J Clin Invest. 118:2609–2619. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Paraiso KHT, Xiang Y, Rebecca VW, Abel EV, Chen YA, Munko AC, Wood E, Fedorenko IV, Sondak VK, Anderson AR, et al: PTEN loss confers BRAF inhibitor resistance to melanoma cells through the suppression of BIM expression. Cancer Res. 71:2750–2760. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Maio M, Grob JJ, Aamdal S, Bondarenko I, Robert C, Thomas L, Garbe C, Chiarion-Sileni V, Testori A, Chen TT, et al: Five-year survival rates for treatment-naive patients with advanced melanoma who received ipilimumab plus dacarbazine in a phase III trial. J Clin Oncol. 33:1191–1196. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Eggermont AMM, Chiarion-Sileni V, Grob JJ, Dummer R, Wolchok JD, Schmidt H, Hamid O, Robert C, Ascierto PA, Richards JM, et al: Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. N Engl J Med. 375:1845–1855. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Ascierto PA, Del Vecchio M, Robert C, Mackiewicz A, Chiarion-Sileni V, Arance A, Lebbé C, Bastholt L, Hamid O, Rutkowski P, et al: Ipilimumab 10 mg/kg versus ipilimumab 3 mg/kg in patients with unresectable or metastatic melanoma: A randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 18:611–622. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, Hassel JC, Rutkowski P, McNeil C, Kalinka-Warzocha E, et al: Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 372:320–330. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Weber JS, D'Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, Hoeller C, Khushalani NI, Miller WH Jr, Lao CD, et al: Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 16:375–384. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Larkin J, Minor D, D'Angelo S, Neyns B, Smylie M, Miller WH Jr, Gutzmer R, Linette G, Chmielowski B, Lao CD, et al: Overall survival in patients with advanced melanoma who received nivolumab versus investigator's choice chemotherapy in CheckMate 037: A randomized, controlled, open-label phase III trial. J Clin Oncol. 36:383–390. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Weber J, Mandala M, Del Vecchio M, Gogas HJ, Arance AM, Cowey CL, Dalle S, Schenker M, Chiarion-Sileni V, Marquez-Rodas I, et al: Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 377:1824–1835. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Ribas A, Puzanov I, Dummer R, Schadendorf D, Hamid O, Robert C, Hodi FS, Schachter J, Pavlick AC, Lewis KD, et al: Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): A randomised, controlled, phase 2 trial. Lancet Oncol. 16:908–918. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Robert C, Ribas A, Schachter J, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil CM, Lotem M, et al: Pembrolizumab versus ipilimumab in advanced melanoma (KEYNOTE-006): Post-hoc 5-year results from an open-label, multicentre, randomised, controlled, phase 3 study. Lancet Oncol. 20:1239–1251. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Schachter J, Ribas A, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M, et al: Pembrolizumab versus ipilimumab for advanced melanoma: Final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet. 390:1853–1862. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Long GV, Atkinson V, Ascierto PA, Robert C, Hassel JC, Rutkowski P, Savage KJ, Taylor F, Coon C, Gilloteau I, et al: Effect of nivolumab on health-related quality of life in patients with treatment-naïve advanced melanoma: Results from the phase III CheckMate 066 study. Ann Oncol. 27:1940–1946. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Schadendorf D, Dummer R, Hauschild A, Robert C, Hamid O, Daud A, van den Eertwegh A, Cranmer L, O'Day S, Puzanov I, et al: Health-related quality of life in the randomised KEYNOTE-002 study of pembrolizumab versus chemotherapy in patients with ipilimumab-refractory melanoma. Eur J Cancer. 67:46–54. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Nosrati A, Tsai KK, Goldinger SM, Tumeh P, Grimes B, Loo K, Algazi AP, Nguyen-Kim TDL, Levesque M, Dummer R, et al: Evaluation of clinicopathological factors in PD-1 response: derivation and validation of a prediction scale for response to PD-1 monotherapy. Br J Cancer. 116:1141–1147. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Zhang Y, Liu B, Kotenko S and Li W: Prognostic value of neutrophil-lymphocyte ratio and lactate dehydrogenase in melanoma patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis. Medicine (Baltimore). 101(e29536)2022.PubMed/NCBI View Article : Google Scholar | |
|
Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Long GV, Ross MI, Lazar AJ, Faries MB, Kirkwood JM, McArthur GA, et al: Melanoma staging: Evidence-based changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 67:472–492. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Balch CM, Gershenwald JE, Soong SJ, Soong SJ, Thompson JF, Atkins MB, Byrd DR, Buzaid AC, Cochran AJ, Coit DG, et al: Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 27:6199–6206. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Hauschild A, Engel G, Brenner W, Gläser R, Mönig H, Henze E and Christophers E: S100B protein detection in serum is a significant prognostic factor in metastatic melanoma. Oncology. 56:338–344. 1999.PubMed/NCBI View Article : Google Scholar | |
|
Jury CS, McAllister EJ and MacKie RM: Rising levels of serum S100 protein precede other evidence of disease progression in patients with malignant melanoma. Br J Dermatol. 143:269–274. 2000.PubMed/NCBI View Article : Google Scholar | |
|
Mårtenson ED, Hansson LO, Nilsson B, von Schoultz E, Månsson Brahme E, Ringborg U and Hansson J: Serum S-100b protein as a prognostic marker in malignant cutaneous melanoma. J Clin Oncol. 19:824–831. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Janka EA, Várvölgyi T, Sipos Z, Soós A, Hegyi P, Kiss S, Dembrovszky F, Csupor D, Kéringer P, Pécsi D, et al: Predictive performance of serum S100B versus LDH in melanoma patients: A systematic review and meta-analysis. Front Oncol. 11(772165)2021.PubMed/NCBI View Article : Google Scholar | |
|
Friedman RC, Farh KKH, Burge CB and Bartel DP: Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 19:92–105. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Lim LP, Glasner ME, Yekta S, Burge CB and Bartel DP: Vertebrate microRNA genes. Science. 299(1540)2003.PubMed/NCBI View Article : Google Scholar | |
|
Lagos-Quintana M, Rauhut R, Lendeckel W and Tuschl T: Identification of novel genes coding for small expressed RNAs. Science. 294:853–858. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Lau NC, Lim LP, Weinstein EG and Bartel DP: An abundant class of tiny RNAs with probable regulatory roles in Caenorhabditis elegans. Science. 294:858–862. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Lee RC and Ambros V: An extensive class of small RNAs in Caenorhabditis elegans. Science. 294:862–864. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Pfeffer SR, Grossmann KF, Cassidy PB, Yang CH, Fan M, Kopelovich L, Leachman SA and Pfeffer LM: Detection of exosomal miRNAs in the plasma of melanoma patients. J Clin Med Res. 4:2012–2027. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Lin N, Zhou Y, Lian X and Tu Y: Expression of microRNA-106b and its clinical significance in cutaneous melanoma. Genet Mol Res. 14:16379–16385. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Friedman EB, Shang S, de Miera EVS, Fog JU, Teilum MW, Ma MW, Berman RS, Shapiro RL, Pavlick AC, Hernando E, et al: Serum microRNAs as biomarkers for recurrence in melanoma. J Transl Med. 10(155)2012.PubMed/NCBI View Article : Google Scholar | |
|
Wróblewska JP, Lach MS, Ustaszewski A, Kulcenty K, Ibbs M, Jagiełło I, Suchorska WM and Marszałek A: The potential role of selected miRNA in uveal melanoma primary tumors as early biomarkers of disease progression. Genes (Basel). 11(271)2020.PubMed/NCBI View Article : Google Scholar | |
|
Tsao SCH, Weiss J, Hudson C, Christophi C, Cebon J, Behren A and Dobrovic A: Monitoring response to therapy in melanoma by quantifying circulating tumour DNA with droplet digital PCR for BRAF and NRAS mutations. Sci Rep. 5(11198)2015.PubMed/NCBI View Article : Google Scholar | |
|
Girotti MR, Gremel G, Lee R, Galvani E, Rothwell D, Viros A, Mandal AK, Lim KH, Saturno G, Furney SJ, et al: Application of sequencing, liquid biopsies, and patient-derived xenografts for personalized medicine in melanoma. Cancer Discov. 6:286–299. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Clark WH Jr, Elder DE, Guerry D IV, Braitman LE, Trock BJ, Schultz D, Synnestvedt M and Halpern AC: Model predicting survival in stage I melanoma based on tumor progression. J Natl Cancer Inst. 81:1893–1904. 1989.PubMed/NCBI View Article : Google Scholar | |
|
Clemente CG, Mihm MC Jr, Bufalino R, Zurrida S, Collini P and Cascinelli N: Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer. 77:1303–1310. 1996.PubMed/NCBI View Article : Google Scholar | |
|
Mandalà M and Massi D: Tissue prognostic biomarkers in primary cutaneous melanoma. Virchows Arch. 464:265–281. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Balch CM, Murad TM, Soong SJ, Ingalls AL, Halpern NB and Maddox WA: A multifactorial analysis of melanoma: Prognostic histopathological features comparing Clark's and Breslow's staging methods. Ann Surg. 188:732–742. 1978.PubMed/NCBI View Article : Google Scholar | |
|
Lattanzi M, Lee Y, Simpson D, Moran U, Darvishian F, Kim RH, Hernando E, Polsky D, Hanniford D, Shapiro R, et al: Primary melanoma histologic subtype: Impact on survival and response to therapy. J Natl Cancer Inst. 111:180–188. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Robinson E, Kulkarni PM, Pradhan JS, Gartrell RD, Yang C, Acs B, Rohr B, Phelps R, Ferringer T, Horst B, et al: Prediction of distant melanoma recurrence from primary tumor digital H&E images using deep learning. J Clin Orthod. 37 (15 Suppl)(S9577)2019. | |
|
Lehmann JM, Holzmann B, Breitbart EW, Schmiegelow P, Riethmüller G and Johnson JP: Discrimination between benign and malignant cells of melanocytic lineage by two novel antigens, a glycoprotein with a molecular weight of 113,000 and a protein with a molecular weight of 76,000. Cancer Res. 47:841–845. 1987.PubMed/NCBI | |
|
Lei X, Guan CW, Song Y and Wang H: The multifaceted role of CD146/MCAM in the promotion of melanoma progression. Cancer Cell Int. 15(3)2015.PubMed/NCBI View Article : Google Scholar | |
|
Pacifico MD, Grover R, Richman PI, Daley FM, Buffa F and Wilson GD: Development of a tissue array for primary melanoma with long-term follow-up: Discovering melanoma cell adhesion molecule as an important prognostic marker. Plast Reconstr Surg. 115:367–375. 2005.PubMed/NCBI View Article : Google Scholar | |
|
Weinstein D, Leininger J, Hamby C and Safai B: Diagnostic and prognostic biomarkers in melanoma. J Clin Aesthet Dermatol. 7:13–24. 2014.PubMed/NCBI | |
|
Gimotty PA, Van Belle P, Elder DE, Murry T, Montone KT, Xu X, Hotz S, Raines S, Ming ME, Wahl P and Guerry D: Biologic and prognostic significance of dermal Ki67 expression, mitoses, and tumorigenicity in thin invasive cutaneous melanoma. J Clin Oncol. 23:8048–8056. 2005.PubMed/NCBI View Article : Google Scholar | |
|
Ladstein RG, Bachmann IM, Straume O and Akslen LA: Ki-67 expression is superior to mitotic count and novel proliferation markers PHH3, MCM4 and mitosin as a prognostic factor in thick cutaneous melanoma. BMC Cancer. 10(140)2010.PubMed/NCBI View Article : Google Scholar | |
|
Tu TJ, Ma MW, Monni S, Rose AE, Yee H, Darvishian F, Polsky D, Berman RS, Shapiro RL, Pavlick AC, et al: A high proliferative index of recurrent melanoma is associated with worse survival. Oncology. 80:181–187. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Kahn HJ, Bailey D and Marks A: Monoclonal antibody D2-40, a new marker of lymphatic endothelium, reacts with Kaposi's sarcoma and a subset of angiosarcomas. Mod Pathol. 15:434–440. 2002.PubMed/NCBI View Article : Google Scholar | |
|
Kahn HJ and Marks A: A new monoclonal antibody, D2-40, for detection of lymphatic invasion in primary tumors. Lab Invest. 82:1255–1257. 2002.PubMed/NCBI View Article : Google Scholar | |
|
Niakosari F, Kahn HJ, McCready D, Ghazarian D, Rotstein LE, Marks A, Kiss A and From L: Lymphatic invasion identified by monoclonal antibody D2-40, younger age, and ulceration: Predictors of sentinel lymph node involvement in primary cutaneous melanoma. Arch Dermatol. 144:462–467. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Rittling SR and Chambers AF: Role of osteopontin in tumour progression. Br J Cancer. 90:1877–1881. 2004.PubMed/NCBI View Article : Google Scholar | |
|
Rudland PS, Platt-Higgins A, El-Tanani M, Silva Rudland S, Barraclough R, Winstanley JH, Howitt R and West CR: Prognostic significance of the metastasis-associated protein osteopontin in human breast cancer. Cancer Res. 62:3417–3427. 2002.PubMed/NCBI | |
|
Pan HW, Ou YH, Peng SY, Liu SH, Lai PL, Lee PH, Sheu JC, Chen CL and Hsu HC: Overexpression of osteopontin is associated with intrahepatic metastasis, early recurrence, and poorer prognosis of surgically resected hepatocellular carcinoma. Cancer. 98:119–127. 2003.PubMed/NCBI View Article : Google Scholar | |
|
Rangel J, Nosrati M, Torabian S, Shaikh L, Leong SP, Haqq C, Miller JR II, Sagebiel RW and Kashani-Sabet M: Osteopontin as a molecular prognostic marker for melanoma. Cancer. 112:144–150. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Thomas NE, Edmiston SN, Alexander A, Groben PA, Parrish E, Kricker A, Armstrong BK, Anton-Culver H, Gruber SB, From L, et al: Association between NRAS and BRAF mutational status and melanoma-specific survival among patients with higher-risk primary melanoma. JAMA Oncol. 1:359–368. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Cirenajwis H, Lauss M, Ekedahl H, Törngren T, Kvist A, Saal LH, Olsson H, Staaf J, Carneiro A, Ingvar C, et al: NF1-mutated melanoma tumors harbor distinct clinical and biological characteristics. Mol Oncol. 11:438–451. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Schumacher TN and Schreiber RD: Neoantigens in cancer immunotherapy. Science. 348:69–74. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Van Allen EM, Miao D, Schilling B, Shukla SA, Blank C, Zimmer L, Sucker A, Hillen U, Foppen MHG, Goldinger SM, et al: Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science. 350:207–211. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Snyder A, Makarov V, Merghoub T, Yuan J, Zaretsky JM, Desrichard A, Walsh LA, Postow MA, Wong P, Ho TS, et al: Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 371:2189–2199. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Samstein RM, Lee CH, Shoushtari AN, Hellmann MD, Shen R, Janjigian YY, Barron DA, Zehir A, Jordan EJ, Omuro A, et al: Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet. 51:202–206. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Johnson DB, Lovly CM, Flavin M, Panageas KS, Ayers GD, Zhao Z, Iams WT, Colgan M, DeNoble S, Terry CR, et al: Impact of NRAS mutations for patients with advanced melanoma treated with immune therapies. Cancer Immunol Res. 3:288–295. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Johnson DB, Bordeaux J, Kim JY, Vaupel C, Rimm DL, Ho TH, Joseph RW, Daud AI, Conry RM, Gaughan EM, et al: Quantitative spatial profiling of PD-1/PD-L1 interaction and HLA-DR/IDO-1 predicts improved outcomes of anti-PD-1 therapies in metastatic melanoma. Clin Cancer Res. 24:5250–2560. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Johnson DB, Estrada MV, Salgado R, Sanchez V, Doxie DB, Opalenik SR, Vilgelm AE, Feld E, Johnson AS, Greenplate AR, et al: Melanoma-specific MHC-II expression represents a tumour-autonomous phenotype and predicts response to anti-PD-1/PD-L1 therapy. Nat Commun. 7(10582)2016.PubMed/NCBI View Article : Google Scholar | |
|
Rodig SJ, Gusenleitner D, Jackson DG, Gjini E, Giobbie-Hurder A, Jin C, Chang H, Lovitch SB, Horak C, Weber JS, et al: MHC proteins confer differential sensitivity to CTLA-4 and PD-1 blockade in untreated metastatic melanoma. Sci Transl Med. 10(eaar3342)2018.PubMed/NCBI View Article : Google Scholar | |
|
Chowell D, Morris LGT, Grigg CM, Weber JK, Samstein RM, Makarov V, Kuo F, Kendall SM, Requena D, Riaz N, et al: Patient HLA class I genotype influences cancer response to checkpoint blockade immunotherapy. Science. 359:582–587. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Sanlorenzo M, Vujic I, Floris A, Novelli M, Gammaitoni L, Giraudo L, Macagno M, Leuci V, Rotolo R, Donini C, et al: BRAF and MEK inhibitors increase PD-1-positive melanoma cells leading to a potential lymphocyte-independent synergism with anti-PD-1 antibody. Clin Cancer Res. 24:3377–3385. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Eggermont AMM, Blank CU, Mandala M, Long GV, Atkinson V, Dalle S, Haydon A, Lichinitser M, Khattak A, Carlino MS, et al: Adjuvant pembrolizumab versus placebo in resected stage III melanoma. N Engl J Med. 378:1789–1801. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Rimm DL, Han G, Taube JM, Yi ES, Bridge JA, Flieder DB, Homer R, West WW, Wu H, Roden AC, et al: A prospective, multi-institutional, pathologist-based assessment of 4 immunohistochemistry assays for PD-L1 expression in non-small cell lung cancer. JAMA Oncol. 3:1051–1058. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Rizk EM, Gartrell RD, Barker LW, Esancy CL, Finkel GG, Bordbar DD and Saenger YM: Prognostic and predictive immunohistochemistry-based biomarkers in cancer and immunotherapy. Hematol Oncol Clin North Am. 33:291–299. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Harel M, Ortenberg R, Varanasi SK, Mangalhara KC, Mardamshina M, Markovits E, Baruch EN, Tripple V, Arama-Chayoth M, Greenberg E, et al: Proteomics of melanoma response to immunotherapy reveals mitochondrial dependence. Cell. 179:236–250.e18. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Zhou X, Yu S, Zhao DM, Harty JT, Badovinac VP and Xue HH: Differentiation and persistence of memory CD8(+) T cells depend on T cell factor 1. Immunity. 33:229–240. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Kratchmarov R, Magun AM and Reiner SL: TCF1 expression marks self-renewing human CD8+ T cells. Blood Adv. 2:1685–1690. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Im SJ, Hashimoto M, Gerner MY, Lee J, Kissick HT, Burger MC, Shan Q, Hale JS, Lee J, Nasti TH, et al: Defining CD8+ T cells that provide the proliferative burst after PD-1 therapy. Nature. 537:417–421. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Sade-Feldman M, Yizhak K, Bjorgaard SL, Ray JP, de Boer CG, Jenkins RW, Lieb DJ, Chen JH, Frederick DT, Barzily-Rokni M, et al: Defining T cell states associated with response to checkpoint immunotherapy in melanoma. Cell. 175:998–1013.e20. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Hugo W, Zaretsky JM, Sun L, Song C, Moreno BH, Hu-Lieskovan S, Berent-Maoz B, Pang J, Chmielowski B, Cherry G, et al: Genomic and transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell. 165:35–44. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Ott PA, Bang YJ, Piha-Paul SA, Razak ARA, Bennouna J, Soria JC, Rugo HS, Cohen RB, O'Neil BH, Mehnert JM, et al: T-cell-inflamed gene-expression profile, programmed death ligand 1 expression, and tumor mutational burden predict efficacy in patients treated with pembrolizumab across 20 cancers: KEYNOTE-028. J Clin Oncol. 37:318–327. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Ayers M, Lunceford J, Nebozhyn M, Murphy E, Loboda A, Kaufman DR, Albright A, Cheng JD, Kang SP, Shankaran V, et al: IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest. 127:2930–2940. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Pinato DJ, Howlett S, Ottaviani D, Urus H, Patel A, Mineo T, Brock C, Power D, Hatcher O, Falconer A, et al: Association of prior antibiotic treatment with survival and response to immune checkpoint inhibitor therapy in patients with cancer. JAMA Oncol. 5:1774–1778. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Yang H, Xia L, Chen J, Zhang S, Martin V, Li Q, Lin S, Chen J, Calmette J, Lu M, et al: Stress-glucocorticoid-TSC22D3 axis compromises therapy-induced antitumor immunity. Nat Med. 25:1428–1441. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Altan-Bonnet G and Mukherjee R: Cytokine-mediated communication: A quantitative appraisal of immune complexity. Nat Rev Immunol. 19:205–217. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Eisenring M, vom Berg J, Kristiansen G, Saller E and Becher B: IL-12 initiates tumor rejection via lymphoid tissue-inducer cells bearing the natural cytotoxicity receptor NKp46. Nat Immunol. 11:1030–1038. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Cristiani CM, Capone M, Garofalo C, Madonna G, Mallardo D, Tuffanelli M, Vanella V, Greco M, Foti DP, Viglietto G, et al: Altered frequencies and functions of innate lymphoid cells in melanoma patients are modulated by immune checkpoints inhibitors. Front Immunol. 13(811131)2002.PubMed/NCBI View Article : Google Scholar | |
|
Joshi K, Atwal D, Ravilla R, Pandey Y, Yarlagadda N, Kakadia S, Makhoul I, Hutchins L and Mahmoud F: Immunotherapy outcomes in advanced melanoma in relation to age. Perm J. 24(19.093)2020.PubMed/NCBI View Article : Google Scholar | |
|
Seidel JA, Otsuka A and Kabashima K: Anti-PD-1 and anti-CTLA-4 therapies in cancer: Mechanisms of action, efficacy, and limitations. Front Oncol. 8(86)2018.PubMed/NCBI View Article : Google Scholar | |
|
Wei SC, Duffy CR and Allison JP: Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 8:1069–1086. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Jang SR, Nikita N, Banks J, Keith SW, Johnson JM, Wilson M and Lu-Yao G: Association between sex and immune checkpoint inhibitor outcomes for patients with melanoma. JAMA Netw Open. 4(e2136823)2021.PubMed/NCBI View Article : Google Scholar | |
|
Anstadt EJ, Chu B, Yegya-Raman N, Han X, Doucette A, Poirier K, Mohiuddin JJ, Maity A, Facciabene A, Amaravadi RK, et al: Moderate colitis not requiring intravenous steroids is associated with improved survival in stage IV melanoma after anti-CTLA4 monotherapy, but not combination therapy. Oncologist. 27:799–808. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Jansen YJL, Rozeman EA, Mason R, Goldinger SM, Geukes Foppen MH, Hoejberg L, Schmidt H, van Thienen JV, Haanen JBAG, Tiainen L, et al: Discontinuation of anti-PD-1 antibody therapy in the absence of disease progression or treatment limiting toxicity: Clinical outcomes in advanced melanoma. Ann Oncol. 30:1154–1161. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Robert C, Ribas A, Hamid O, Daud A, Wolchok JD, Joshua AM, Hwu WJ, Weber JS, Gangadhar TC, Joseph RW, et al: Durable complete response after discontinuation of pembrolizumab in patients with metastatic melanoma. J Clin Orthod. 36:1668–1674. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Betof Warner A, Palmer JS, Shoushtari AN, Goldman DA, Panageas KS, Hayes SA, Bajwa R, Momtaz P, Callahan MK, Wolchok JD, et al: Long-term outcomes and responses to retreatment in patients with melanoma treated with PD-1 blockade. J Clin Oncol. 38:1655–1663. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Waterhouse DM, Garon EB, Chandler J, McCleod M, Hussein M, Jotte R, Horn L, Daniel DB, Keogh G, Creelan B, et al: Continuous versus 1-year fixed-duration nivolumab in previously treated advanced non-small-cell lung cancer: CheckMate 153. J Clin Orthod. 38:3863–3873. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Wang PF, Chen Y, Song SY, Wang TJ, Ji WJ, Li SW, Liu N and Yan CX: Immune-related adverse events associated with anti-PD-1/PD-L1 treatment for malignancies: A meta-analysis. Front Pharmacol. 8(730)2017.PubMed/NCBI View Article : Google Scholar | |
|
Santini FC, Rizvi H, Plodkowski AJ, Ni A, Lacouture ME, Gambarin-Gelwan M, Wilkins O, Panora E, Halpenny DF, Long NM, et al: Safety and efficacy of re-treating with immunotherapy after immune-related adverse events in patients with NSCLC. Cancer Immunol Res. 6:1093–1099. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Lebbé C, Meyer N, Mortier L, Marquez-Rodas I, Robert C, Rutkowski P, Menzies AM, Eigentler T, Ascierto PA, Smylie M, et al: Evaluation of two dosing regimens for nivolumab in combination with ipilimumab in patients with advanced melanoma: Results from the phase IIIb/IV CheckMate 511 trial. J Clin Oncol. 37:867–875. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Tarhini AA, Lee SJ, Hodi FS, Rao UNM, Cohen GI, Hamid O, Hutchins LF, Sosman JA, Kluger HM, Eroglu Z, et al: Phase III study of adjuvant ipilimumab (3 or 10 mg/kg) versus high-dose interferon alfa-2b for resected high-risk melanoma: North American intergroup E1609. J Clin Oncol. 38:567–575. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Betof AS, Nipp RD, Giobbie-Hurder A, Johnpulle RAN, Rubin K, Rubinstein SM, Flaherty KT, Lawrence DP, Johnson DB and Sullivan RJ: Impact of age on outcomes with immunotherapy for patients with melanoma. Oncologist. 22:963–971. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Zamami Y, Niimura T, Okada N, Koyama T, Fukushima K, Izawa-Ishizawa Y and Ishizawa K: Factors associated with immune checkpoint inhibitor-related myocarditis. JAMA Oncol. 5:1635–1637. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Tan MH, Iyengar R, Mizokami-Stout K, Yentz S, MacEachern MP, Shen LY, Redman B and Gianchandani R: Spectrum of immune checkpoint inhibitors-induced endocrinopathies in cancer patients: A scoping review of case reports. Clin Diabetes Endocrinol. 5(1)2019.PubMed/NCBI View Article : Google Scholar | |
|
Wright JJ, Powers AC and Johnson DB: Endocrine toxicities of immune checkpoint inhibitors. Nat Rev Endocrinol. 17:389–399. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Minkis K, Garden BC, Wu S, Pulitzer MP and Lacouture ME: The risk of rash associated with ipilimumab in patients with cancer: A systematic review of the literature and meta-analysis. J Am Acad Dermatol. 69:e121–e128. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Coleman E, Ko C, Dai F, Tomayko MM, Kluger H and Leventhal JS: Inflammatory eruptions associated with immune checkpoint inhibitor therapy: A single-institution retrospective analysis with stratification of reactions by toxicity and implications for management. J Am Acad Dermatol. 80:990–997. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Sibaud V, Meyer N, Lamant L, Vigarios E, Mazieres J and Delord JP: Dermatologic complications of anti-PD-1/PD-L1 immune checkpoint antibodies. Curr Opin Oncol. 28:254–263. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Sibaud V: Dermatologic reactions to immune checkpoint inhibitors: Skin toxicities and immunotherapy. Am J Clin Dermatol. 19:345–361. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Inno A, Metro G, Bironzo P, Grimaldi AM, Grego E, Di Nunno V, Picasso V, Massari F and Gori S: Pathogenesis, clinical manifestations and management of immune checkpoint inhibitors toxicity. Tumori. 103:405–421. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Kumar V, Chaudhary N, Garg M, Floudas CS, Soni P and Chandra AB: Current diagnosis and management of immune related adverse events (irAEs) Induced by immune checkpoint inhibitor therapy. Front Pharmacol. 8(49)2017.PubMed/NCBI View Article : Google Scholar | |
|
Bryce J and Boers-Doets CB: Non-rash dermatologic adverse events related to targeted therapies. Semin Oncol Nurs. 30:155–168. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Geisler AN, Phillips GS, Barrios DM, Wu J, Leung DYM, Moy AP, Kern JA and Lacouture ME: Immune checkpoint inhibitor-related dermatologic adverse events. J Am Acad Dermatol. 83:1255–1268. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Tewalt EF, Cohen JN, Rouhani SJ, Guidi CJ, Qiao H, Fahl SP, Conaway MR, Bender TP, Tung KS, Vella AT, et al: Lymphatic endothelial cells induce tolerance via PD-L1 and lack of costimulation leading to high-level PD-1 expression on CD8 T cells. Blood. 120:4772–4782. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Sano T, Uhara H, Mikoshiba Y, Kobayashi A, Uchiyama R, Tateishi K, Yamamoto H and Okuyama R: Nivolumab-induced organizing pneumonia in a melanoma patient. Jpn J Clin Oncol. 46:270–272. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Nakashima K, Naito T, Omori S, Yoshikawa S, Endo M, Kiyohara Y and Takahashi T: Organizing pneumonia induced by nivolumab in a patient with metastatic melanoma. J Thorac Oncol. 11:432–433. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Koelzer VH, Rothschild SI, Zihler D, Wicki A, Willi B, Willi N, Voegeli M, Cathomas G, Zippelius A and Mertz KD: Systemic inflammation in a melanoma patient treated with immune checkpoint inhibitors-an autopsy study. J Immunother Cancer. 4(13)2016.PubMed/NCBI View Article : Google Scholar | |
|
Watanabe S, Kimura H, Takato H, Waseda Y, Hara J, Sone T, Abo M, Maeda S, Matsushita T and Kasahara K: Severe pneumonitis after nivolumab treatment in a patient with melanoma. Allergol Int. 65:487–489. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Nishino M, Sholl LM, Hatabu H, Ramaiya NH and Hodi FS: Anti-PD-1-related pneumonitis during cancer immunotherapy. N Engl J Med. 373:288–290. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Mir MA: T-cell costimulation and its applications in diseases. Dev Costimulatory Mol Immunother Dis. 29:255–292. 2015. | |
|
Tarazona R, Duran E and Solana R: Natural killer cell recognition of melanoma: New clues for a more effective immunotherapy. Front Immunol. 6(649)2015.PubMed/NCBI View Article : Google Scholar | |
|
Rieth J and Subramanian S: Mechanisms of intrinsic tumor resistance to immunotherapy. Int J Mol Sci. 19(1340)2018.PubMed/NCBI View Article : Google Scholar | |
|
Fisher DT, Appenheimer MM and Evans SS: The two faces of IL-6 in the tumor microenvironment. Semin Immunol. 26:38–47. 2014.PubMed/NCBI View Article : Google Scholar | |
|
O'Donnell JS, Long GV, Scolyer RA, Teng MWL and Smyth MJ: Resistance to PD1/PDL1 checkpoint inhibition. Cancer Treat Rev. 52:71–81. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Vander Heiden MG, Cantley LC and Thompson CB: Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science. 324:1029–1033. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Ahn CS and Metallo CM: Mitochondria as biosynthetic factories for cancer proliferation. Cancer Metab. 3(1)2015.PubMed/NCBI View Article : Google Scholar | |
|
O'Donnell JS, Teng MWL and Smyth MJ: Cancer immunoediting and resistance to T cell-based immunotherapy. Nat Rev Clin Oncol. 16:151–167. 2019.PubMed/NCBI View Article : Google Scholar | |
|
DeBerardinis RJ and Chandel NS: Fundamentals of cancer metabolism. Sci Adv. 2(e1600200)2016.PubMed/NCBI View Article : Google Scholar | |
|
Robey IF, Lien AD, Welsh SJ, Baggett BK and Gillies RJ: Hypoxia-inducible factor-1alpha and the glycolytic phenotype in tumors. Neoplasia. 7:324–330. 2005.PubMed/NCBI View Article : Google Scholar | |
|
Franco F, Jaccard A, Romero P, Yu YR and Ho PC: Metabolic and epigenetic regulation of T-cell exhaustion. Nat Metab. 2:1001–1012. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Jiang Y, Li Y and Zhu B: T-cell exhaustion in the tumor microenvironment. Cell Death Dis. 6(e1792)2015.PubMed/NCBI View Article : Google Scholar | |
|
Sirico M, D'Angelo A, Gianni C, Casadei C, Merloni F and De Giorgi U: Current state and future challenges for PI3K inhibitors in cancer therapy. Cancers (Basel). 15(703)2023.PubMed/NCBI View Article : Google Scholar | |
|
Peng W, Chen JQ, Liu C, Malu S, Creasy C, Tetzlaff MT, Xu C, McKenzie JA, Zhang C, Liang X, et al: Loss of PTEN promotes resistance to T cell-mediated immunotherapy. Cancer Discov. 6:202–216. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Li X, Wenes M, Romero P, Huang SCC, Fendt SM and Ho PC: Navigating metabolic pathways to enhance antitumour immunity and immunotherapy. Nat Rev Clin Oncol. 16:425–441. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Marin-Acevedo JA, Kimbrough EO and Lou Y: Next generation of immune checkpoint inhibitors and beyond. J Hematol Oncol. 14(45)2021.PubMed/NCBI View Article : Google Scholar |