Effect of prothymosin α on neuroplasticity following cerebral ischemia‑reperfusion injury
- Authors:
- Published online on: February 16, 2024 https://doi.org/10.3892/mmr.2024.13183
- Article Number: 59
-
Copyright: © Lee et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Ischemic stroke is a devastating neurological event that occurs when blood flow to the brain is interrupted, leading to neuronal damage and functional impairment. Despite significant advances in acute management and rehabilitation strategies, most stroke survivors still experience significant impairments in motor, sensory, and cognitive function. Effective neurorestorative therapies are essential to promote neural plasticity and facilitate functional recovery (1).
There are three therapeutic approaches suggested to enhance post-stroke functional recovery. First, interventions target common injury mechanisms for various cytoarchitectural damages, including cortical and subcortical, gray and white matter and the neurovascular unit, to reduce the extension of direct or indirect damage to partially injured (penumbral) brain tissues (2–4). The second is to use specialized treatments that enhance neuroplasticity during the subacute phase of ischemic stroke, including promoting neuronal sprouting, myelin regeneration, dendritic spine density, arborization and synaptic connections (5,6). This leads to restoring or compensating functional deficits caused by ischemic stroke by either enhancing the rewiring process for the damaged brain tissues, decreasing the remote injury that may occur distal to the ischemic territory, or even using other intact brain tissues. The third is to introduce pluripotent stem cells into the ischemic brain or enhance the proliferation, migration and differentiation of endogenous progenitor cells into the damaged brain to restoration of neuronal, axonal, and synaptic functions through replenishing and rewiring of the damaged neural network (7,8). Thus, treatment strategies combining neuroplasticity strategies with neuroprotectants have been suggested (7,9).
Prothymosin α (ProT) is a small, ubiquitous protein essential for cell proliferation and survival through its involvement in chromatin remodeling and proapoptotic activity (10). Furthermore, ProT contributes to neuroprotection against cerebral and retinal ischemia by being involved in anti-necrosis, anti-apoptosis, immunomodulation and oxidative stress (11–15). It has been shown that ProT and peptides derived from ProT attenuated infarction volume and blood vessel disruption and improved functional outcomes (16–18). It was therefore hypothesized that ProT may have a role in promoting neuroplasticity following ischemic injury.
The present study aimed to investigate whether ProT improved axonal sprouting and dendrite branching in cultured neurons exposed to oxygen-glucose deprivation and to explore its potential of neuroplasticity effect of underlying mechanisms of neuroplasticity following ischemia-reperfusion injury in mice.
Materials and methods
Animal preparation, anesthesia and monitoring
All animal procedures were conducted following the Taiwan National Institutes of Health guidelines and approved by the Subcommittee on Research-Animal Care of National Cheng Kung University (NCKU) Medical Center (approval no. 109184). Sprague-Dawley rats (weight, 5–6 g; age, 1 day; n=160; obtained from the Laboratory Animal Center of NCKU) both male and female were used for primary cortical neuron culture, while male FVB mice (weight, 20–25 g; age, 6–8 weeks; n=24; mice were obtained from the Laboratory Animal Center of NCKU, and the ProT-overexpressing transgenic mice were generated by Professor Chao-Liang Wu, Department of Biochemistry and Molecular Biology, NCKU) were used for middle cerebral artery (MCA) occlusion surgery. The animals were housed in the Laboratory Animal Center of NCKU under a 12-h light/dark cycle, with an ambient temperature of 20–26°C and humidity maintained at 40–60%. They were provided with free access to food and water. The animals were anesthetized with isoflurane (induction 4–5%, maintenance 1–2%), and body temperature was maintained at 37°C using a thermostatically controlled heating blanket and rectal probe (Harvard Apparatus) during the surgical procedure.
Protein preparation
ProT and ProTΔ nuclear localizing signal (NLS) proteins preparation as previously described (18). The plasmids encoding wild-type ProT and ProTΔNLS with glutathione-transferase (GST) tags were transformed into BL21 E. coli for protein expression. The transformed E. coli cultures were incubated at 37°C in lysogeny broth medium [tryptone (Merck KGaA) 10 g, yeast extract (Sigma-Aldrich; Merck KGaA) 5 g, sodium chloride (J.T. Baker; Thermo Fisher Scientific, Inc.) 5 g; components dissolved in 1 l ddH2O)]. The optical density of the medium at 600 nm (OD600) reached 0.4–0.8. The cultured cells (1 ml) were transferred to 250 ml of fresh culture medium for large-scale protein expression. To induce protein expression, isopropyl β-D-1-thiogalactopyranoside (0.1 M) was added to the culture medium, and the cells were further incubated at 37°C for 5 h. following induction, the cells were lysed using a sonicator and centrifuged (10,000 × g, 4°C, 10 min). The clear supernatant was then purified using a column designed explicitly for GST-tagged proteins (Pierce Glutathione Superflow Agarose; Thermo Fisher Scientific, Inc.). The column was washed with elution buffer (125 mM Tris-HCl, 150 mM sodium chloride, 10 mM reduced glutathione; pH 8.0) and regeneration buffers to ensure efficient purification.
The column was washed with elution buffer and regeneration buffers to ensure efficient purification. The purified protein solution was eluted by gravity flow (flow rate, ≤150 cm/h) with 5 column volumes of elution buffer and centrifuged (700 × g, room temperature, 2 min) using filter tubes with appropriate molecular weight cut-offs. GST-tagged proteins were concentrated using 10-kDa filter tubes, while ProT and ProTΔNLS were concentrated using 30-kDa filter tubes. The protein concentration was adjusted to 100 µg/50 µl, and the samples were stored in a −20°C refrigerator for future use.
Primary cortical neuronal culture
Primary cortical neurons were obtained from the cerebral cortices of 1-day-old Sprague-Dawley rats under deep anesthesia induced by pentobarbital [150 mg/kg; intraperitoneal (IP)]. Following deep anesthesia, the rats were euthanized by decapitation. The cortical tissue was minced and dissociated in a papain solution containing DNase I [0.6 mg/ml papain and DNase I in Hank's Balanced Salt Solution (HBSS)] at 37°C for 30 min. The reaction was stopped with heat-inactivated horse serum (Thermo Fisher Scientific, Inc.), and the cell suspension was centrifuged at 800 × g, 4°C, 5 min and plated onto poly-D-lysine-coated Petri dishes. The dissociated cells were cultured in DMEM with 10% horse serum at 37°C in a humidified incubator with 5% CO2. After 3 h of plating, the culture medium was replaced with a serum-free neurobasal medium containing 25 mM glutamate, 0.5 mM L-glutamine, and 2% B27 supplement (cat. no. 17504-044; Invitrogen; Thermo Fisher Scientific, Inc.). The culture medium was changed every 3 days, and the cultured cells were allowed to grow for ~6-8 days.
Oxygen and glucose deprivation (OGD)
The OGD medium consisted of HBSS without glucose and bubbled with N2 for 30 min. Cultured neurons were then exposed to the OGD medium and transferred to an anaerobic chamber with an N2-enriched atmosphere at 37°C for 2 h. Following the deprivation period, the cultured neurons were incubated in a neuron basal medium under normal incubator conditions (5% CO2 at 37°C).
Transfection of primary neuron cells
To transfect primary neuron cells, 6 cm dishes were used for plating. A solution containing 1 µg of DNA from the ProT plasmid, ProTΔNLS plasmid, or empty pLKO.1-GFP plasmid (sham or OGD groups), along with Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) was prepared by diluting them in 250 µl of neurobasal medium (Invitrogen; Thermo Fisher Scientific, Inc.) for 5 min at room temperature. The DNA and Lipofectamine® 2000 were then mixed and incubated for 20 min at room temperature. Subsequently, the DNA-Lipofectamine® 2000 complexes were added to each well, and the cells were incubated at 37°C for 4 h, after which the medium was replaced with fresh medium. After 24 h, neuron cells were used for the OGD experiment.
Immunofluorescence staining and quantification
Neurons cultured on coverslips were post-fixed in 4% paraformaldehyde in PBS for 5 min at room temperature and rinsed with PBS 3 times. Coverslips were processed with primary antibodies at a dilution of 1:1,000 against MAP-2 (cat. no. sc-390543; Santa Cruz Biotechnology, Inc.) or 1:100 against prothymosin α (2F11; cat. no. ALX-804-486-C100; Enzo Life Sciences, Inc.) at 4°C overnight. Subsequently, an appropriate secondary antibody conjugated with biotin (1:150; cat. no. 115-065-003; Jackson ImmunoResearch Laboratories, Inc.) was added, followed by DTAF-conjugated streptavidin (green; 1:100; cat. no. 016-010-084; Jackson ImmunoResearch Laboratories, Inc.) or Alexa red-conjugated streptavidin (red; 1:100; cat, no. 016-580-084; Jackson ImmunoResearch Laboratories, Inc.). The sections were co-incubated with DAPI (blue; 1:1,000; cat. no. D8417; MilliporeSigma) at room temperature for 10 min. Fluorescent photomicrographs of labeled neurons were captured in at least three fields of view and each result quantified at ×40 magnification using a CoolSNAP-Pro cf digital camera (Media Cybernetics Inc.). The Digital Image Analysis System MCID Elite (version 6.0; Imaging Research Inc.) was employed to assess the relative intensity of ProT. ImageJ software (1.49v, National Institutes of Health) with the Neuron J plugin was utilized to upload MAP-2-stained images for the analysis of the number and length of neuronal dendrite branches.
RNA isolation and PCR
Total RNA was isolated from cultured neurons using TRIzol™ Reagent, (Invitrogen; Thermo Fisher Scientific, Inc.), and cDNA synthesis was performed using High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems; Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. The PCR amplification consisted of an initial denaturation for 5 min at 95°C, followed by 35 cycles of 30 sec denaturation at 95°C, annealing for 45 sec at 58°C and extension for 1 min at 72°C. The final extension step was carried out at 72°C for 10 min. RT-PCR was carried out with specific primers for brain-derived neurotrophic factor (BDNF), 5′-CCTCCTCTGCTCTTTCTGC-′3 (forward) and 5′-TCCCATTACACTTGGTCTCGT-3′ (reverse); GAPDH, 5′-CCAAAGTTGTCATGGATGACC-3′ (forward) and 5′-GTCTTCACCACCATGGAG-3′ (reverse), and the PCR products were separated by 2% agarose gel electrophoresis and visualized using ethidium bromide staining. Gel documentation was performed under UV light for analysis and documentation of band patterns.
Experimental model and grouping
Focal cerebral ischemia was induced by intra-arterial suture occlusion of the proximal right middle cerebral artery (MCA) for 50 min. Briefly, a 4-0 nylon suture with its tip rounded by heating over a flame and subsequently coated with silicone (Merck KGaA) was inserted from the external carotid artery into the internal carotid artery until the tip occluded the origin of the MCA (19,20). Laser-Doppler flowmetry (LDF; Laserflo BMP2; Vasamedics Inc.) was used for local cortical blood perfusion (LCBF) measurement, as previously described (21). The scalp was incised along the midline, and two areas in bilateral parietal bones were thinned 0.5 mm posterior and 7 mm lateral to the bregma to place the LDF probes. Another area in the right parietal bone was thinned 2.0 mm posterior and 2.5 mm lateral to the bregma for additional LCBF measurements. LCBF was measured prior to and during MCA occlusion and expressed as a percentage of the baseline values. Animals were assigned to three groups: i) WT control group (n=7), ii) WT ProT injection group (n=8) and iii) ProT transgene group (n=8). ProT overexpression in transgenic mice has been described (22,23). Briefly, the ProT minigene employed for transgenic mouse production was designated pJ6Ω-ProT. This construct comprised a complete 1.2-kb murine ProT cDNA sequence, under the control of the rat β-actin promoter and SV40 polyadenylation tail. The minigene, isolated from pJ6Ω-ProT through PvuII and ScaI digestions, underwent microinjection into the pronuclei of FVB zygotes. Subsequently, the injected eggs were transferred into the oviducts of pseudopregnant recipients. Genomic DNA from founder mice, obtained via tail biopsies, was subjected to PCR analysis using RAP-f and ProT-r1 primers to confirm the integration of the transgenic ProT minigene. Normal saline or ProT protein (100 µg/kg; IP) was injected upon reperfusion (13,18).
Neurobehavioral testing and body weight measurements
Body weight measurements and neurobehavioral testing were conducted both before the surgery and prior to sacrifice. A total of two neurological grading systems, modified from previous versions (19,24,25), were employed to assess various aspects of neurological function: i) Sensory Test; this examination focused on sensorimotor integration in forelimb placing responses to visual and tactile stimuli. The affected forelimb underwent forward and sideways visual placing tests, with scores assigned to each test as follows: 0, complete immediate placing; 1, incomplete and/or delayed placing (<2 sec); and 2, absence of placing. Additionally, the motor test involved the postural reflex test to evaluate upper body posture while the animal's tail was suspended. Scores for this test were as follows: 0, no observable deficit; 1, forelimb flexion; 2, forelimb flexion and decreased resistance to lateral push; 3, forelimb flexion, decreased resistance to lateral push and unilateral circling; and 4, forelimb flexion, making ambulation difficult or impossible. ii) Animals were also rated using a scale developed by Clark et al (26), with scores ranging 0–28 used for further analysis. Higher scores indicate more severe brain defects caused by brain injury.
Protein extraction and western blot analysis
The brain tissue was removed after the animal was deeply anesthetized (isoflurane 5%; inhalation), and cell lysates were prepared with lysis buffer, containing 1% Triton X-100, 20 mM Tris-HCl (pH 7.5), 150 mM NaCl, 0.5% sodium deoxycholate, 1 mM EDTA and 0.1% SDS, and were centrifuged at 18,000 × g for 60 min at 4°C. Protein concentrations were determined using a BCA protein assay kit (Pierce; Thermo Fisher Scientific, Inc.). Subsequently, 10% SDS-PAGE was used to separate the 25 µg protein samples, which were then transferred onto PVDF microporous membranes. The membranes were blocked with 5% skim milk in TBS −0.05% Tween-20 for 30 min at room temperature and probed with primary antibodies against growth-associated protein-43 (GAP-43; 1:1,000; cat. no. AB5220; Chemicon; Sigma-Aldrich; Merck KGaA), postsynaptic density protein 95 (PSD-95; 1:1,000; cat. no. AB9708; Chemicon, Sigma-Aldrich; Merck KGaA), synaptosomal-associated protein, 25 kDa (SNAP-25; 1:1,000; cat. no. AHP1124; Bio-Rad Laboratories, Inc.) and β-actin (1:10,000; cat. no. ABT264; Chemicon; Sigma-Aldrich; Merck KGaA) overnight at 4°C. Membranes were then incubated with horseradish peroxidase-conjugated immunoglobulin secondary antibody (1:5,000; cat. nos. AP106P and AP182P; Chemicon; Sigma-Aldrich; Merck KGaA) for 30 min at room temperature. Proteins were visualized with an Enhanced Chemiluminescence kit (GE Healthcare Bio-Sciences). Optical densities were measured using Multi Gauge V3.0 (Fuji Photo Film Co., Ltd.) on a Luminescent Image Analyzer (Fujifilm LAS-3000; Fuji Photo Film Co., Ltd.).
Statistical analysis
All data were expressed as the mean ± SD. Paired Students' t-test was used to evaluate the response to a change in conditions, and unpaired Student's t-test/one-way ANOVA with Fisher's protected least significant difference (LSD) and Tukey's post hoc comparison was used to evaluate differences between groups. Neurobehavioral scores were expressed as medians ±95% confidence interval (CI) and analyzed using the Mann-Whitney U test. Data were analyzed using SPSS version 17.0 software (SPSS Inc.). P<0.05 was considered to indicate a statistically significant difference.
Results
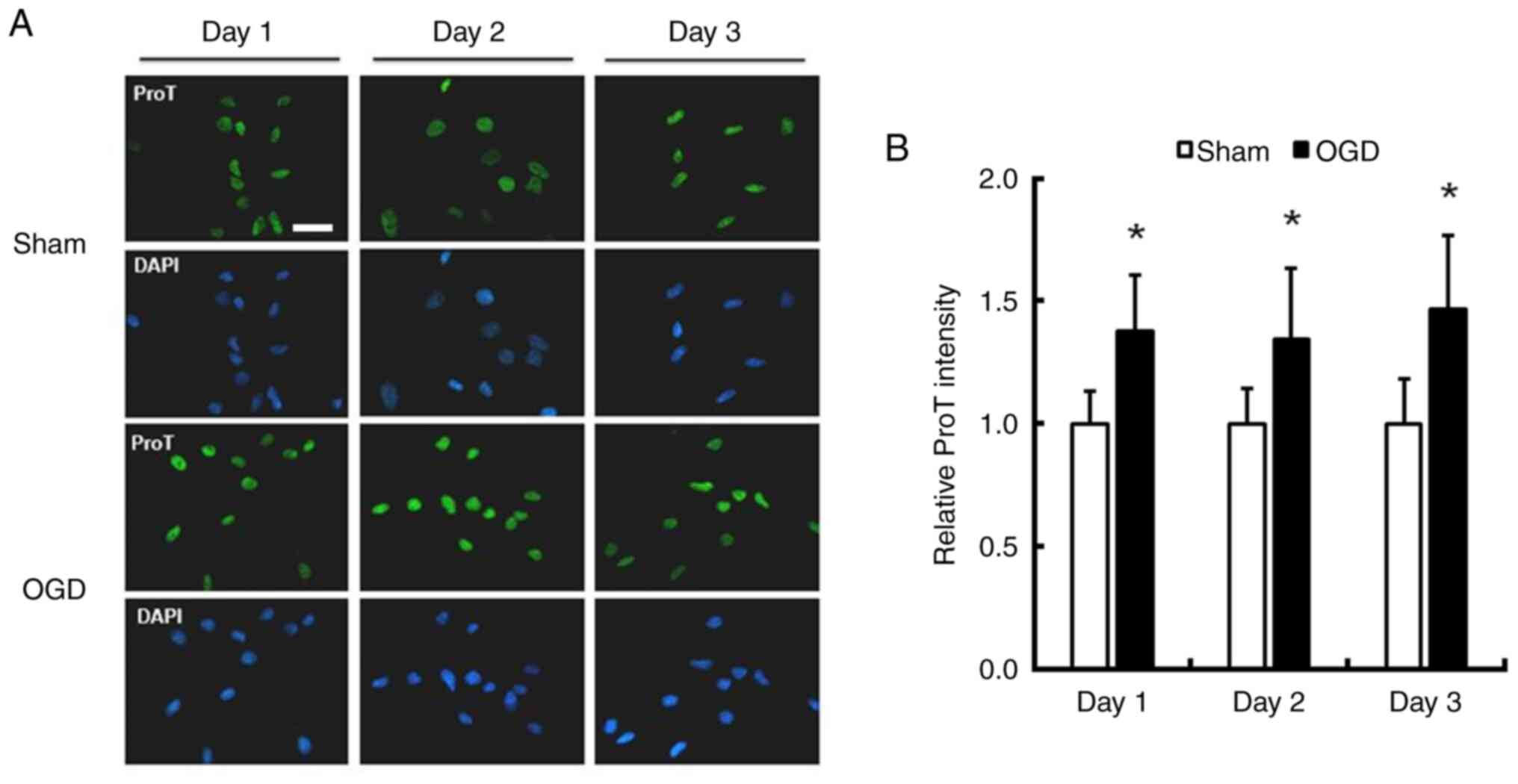
Increased ProT expression in cortical neurons exposed to OGD
To investigate the influence of OGD on ProT protein expression, cortical neurons obtained from 1-day-old rats were cultured for ~1 week. Immunofluorescence staining of ProT/DAPI was performed on cultures exposed to OGD for 1–3 days to assess changes in ProT expression. The intensity of ProT significantly increased by 37.9, 34.2 and 46.5% in cultured neurons 1–3 days after exposure to OGD, respectively (Fig. 1; P<0.05).
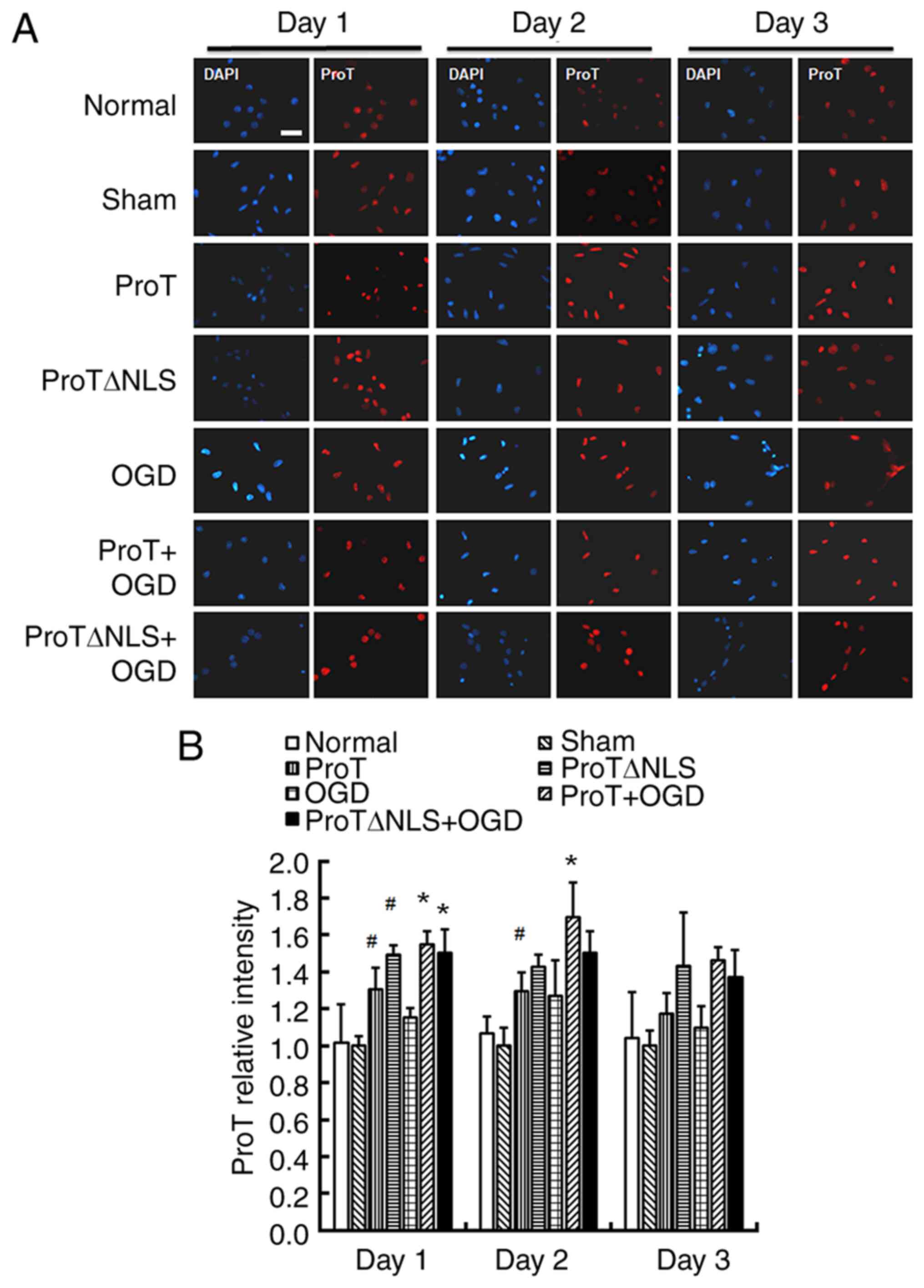
Transfection increases ProT gene expression
To evaluate the effect of ProT on neuronal plasticity in cultured cortical neurons after OGD injury, ProT/ProTΔNLS plasmid DNA transfection was conducted prior to OGD, while the sham and OGD group were transfected with empty plasmid. The sham group did not exhibit an increase in ProT expression compared with the normal group. Immunofluorescence staining of ProT was performed on cultured neurons after OGD for 1–3 days (Fig. 2A). The relative intensity of ProT was significantly increased compared with the sham or the OGD control group (Fig. 2B; see Table SI for more precise data).
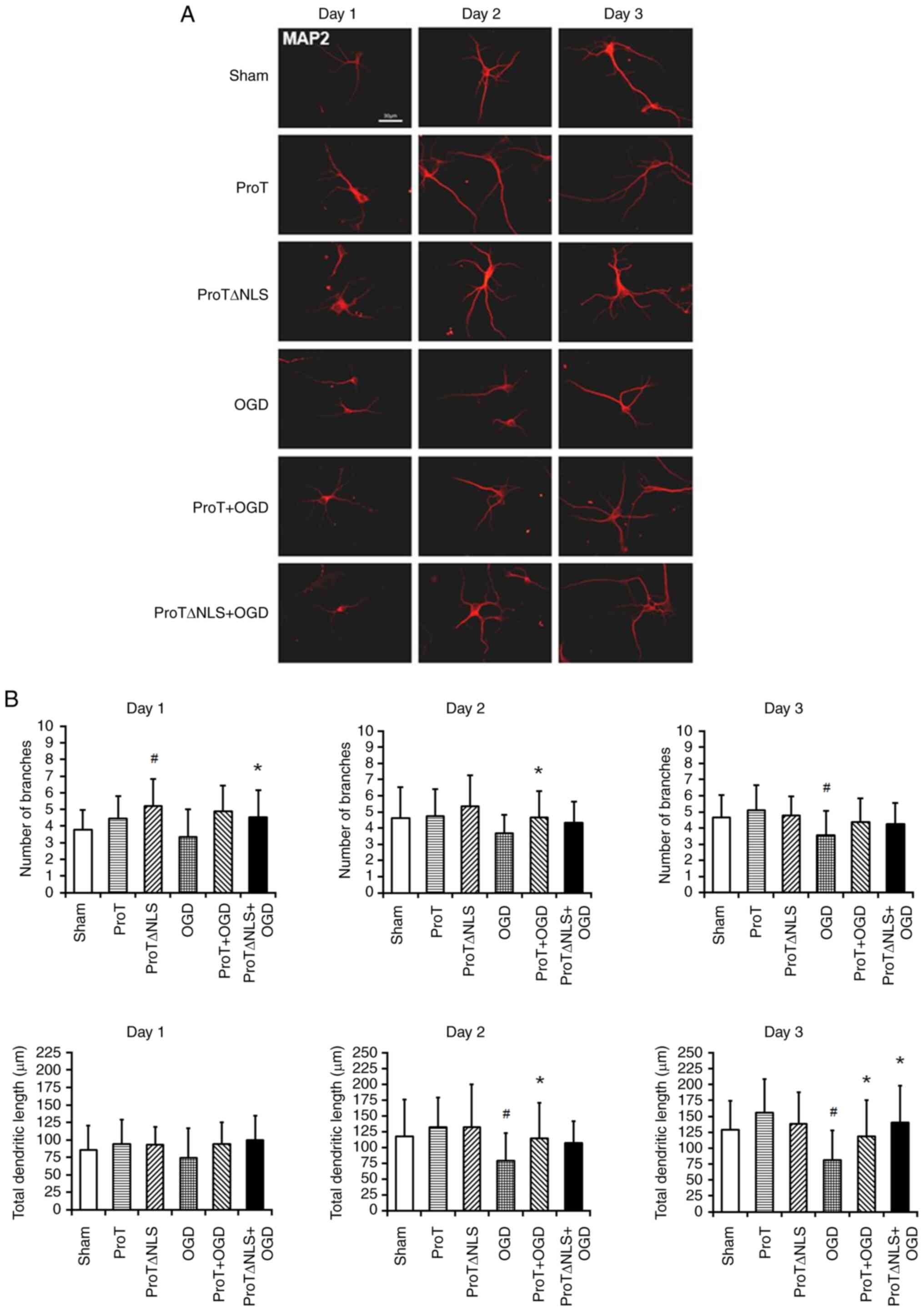
Transfection of the ProT gene increases cultured neuron dendritic arborization following OGD injury
To investigate the direct effect of ProT on neurite plasticity, neurons were transfected with ProT/ProTΔNLS plasmid DNA before being subjected to OGD injury, while the sham and OGD groups were transfected with empty plasmid. The total length of neurites and the number of dendritic branches were quantified by MAP-2 immunofluorescence staining (Fig. 3A). MAP2 isoforms are specialized cytoskeletal proteins found predominantly in neurons, where they are abundant in dendrites and perikarya. This suggests their involvement in shaping and maintaining neuronal morphology as neurons develop. MAP2 is a commonly employed marker for identifying neuronal cells and visualizing dendritic processes (27,28). In the OGD group, neurites exhibited rupture and shortening compared with the sham control, resulting in decreased total length and number of branches. However, compared with the OGD group, transfection with ProT/ProTΔNLS plasmid DNA significantly increased the total length and number of branches, indicating enhanced neurite plasticity in cultured primary cortical neurons following OGD injury (Fig. 3B; Table SII).
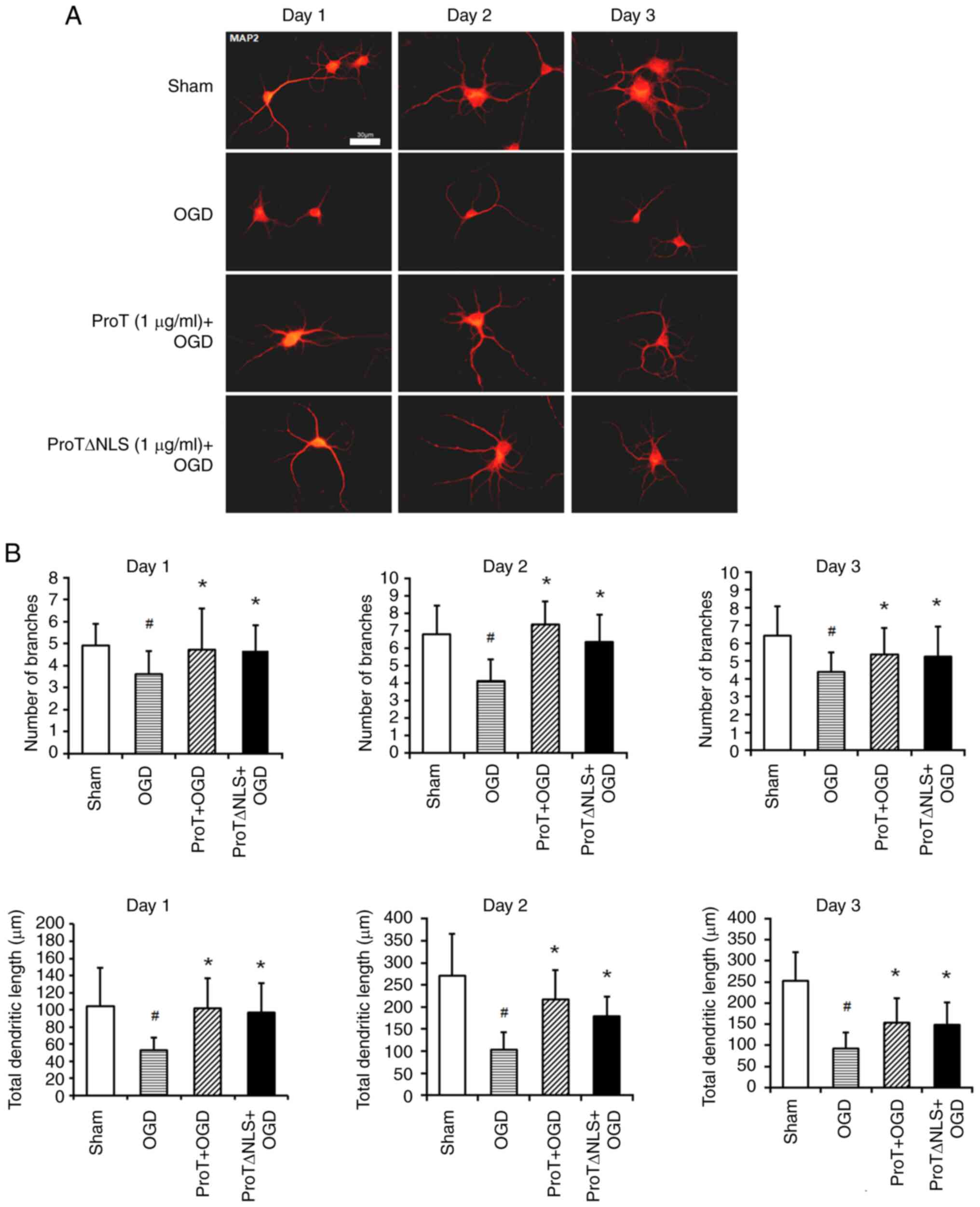
ProT treatment increases cultured neuron dendritic arborization after OGD injury
To ascertain the role of ProT in neuronal plasticity, the cultured neurons were pre-treated with ProT/ProTΔNLS protein before OGD injury. The total length of neurites and the number of dendritic branches were calculated by MAP-2 immunofluorescence staining (Fig. 4A). Compared with the sham control group, in the OGD group, neurites were ruptured and shortened and the total length and number of branches significantly decreased. However, compared with that of the OGD group, the total length and number of branches significantly increased in the ProT/ProTΔNLS protein-treated group upon OGD injury. These data suggested that ProT/ProTΔNLS protein treatment facilitated neurite plasticity in cultured primary cortical neurons after OGD injury (Fig. 4B; Table SIII).
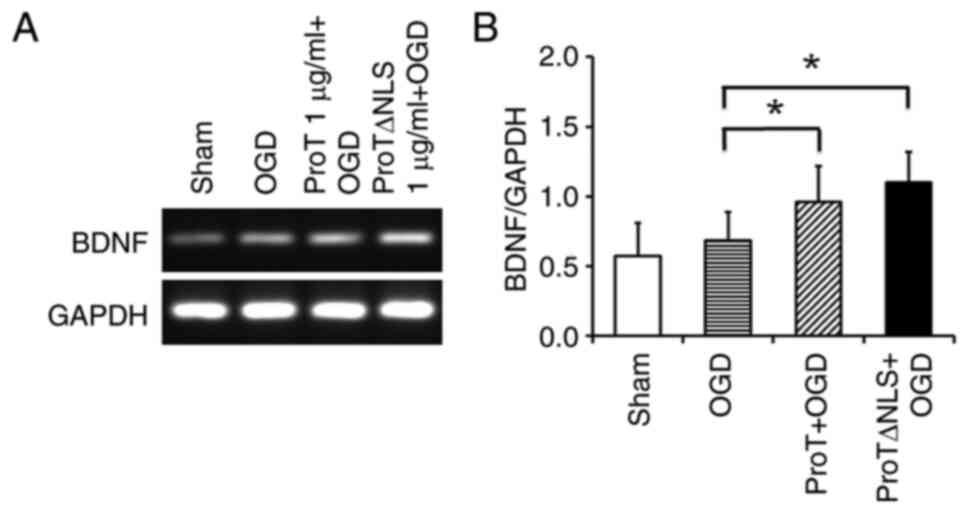
ProT treatment increases BDNF mRNA levels after OGD injury
To examine whether ProT/ProTΔNLS treatment would virtually promote BDNF levels in the neurons after exposure to OGD. Treatment of ProT/ProTΔNLS protein significantly increased the level of BDNF mRNA level by 40.0 and 60.7%, respectively (Fig. 5).
In vivo stroke animal model
To further investigate the underlying mechanism of the neuroplastic effect of ProT in vivo, focal cerebral ischemia was employed on FVB wild-type mice and FVB ProT overexpression in transgenic mice by intra-arterial suture occlusion of the proximal right MCA for 50 min. LCBF was measured prior to and during the MCA occlusion and after the onset of reperfusion (Table SIV). Body temperature was kept constantly at 37°C.
ProT improves neurologic behavior score
To evaluate whether ProT treatment improves neurobehavioral outcomes, a neurologic behavior test was conducted. The ProT-treated and ProT overexpression in transgenic mice groups had a less severe neurologic behavior score than the control group, especially significant in the 28-point clinical scale (Table I) (26). This result indicated that ProT ameliorated neurobehavioral recovery after ischemic insults.
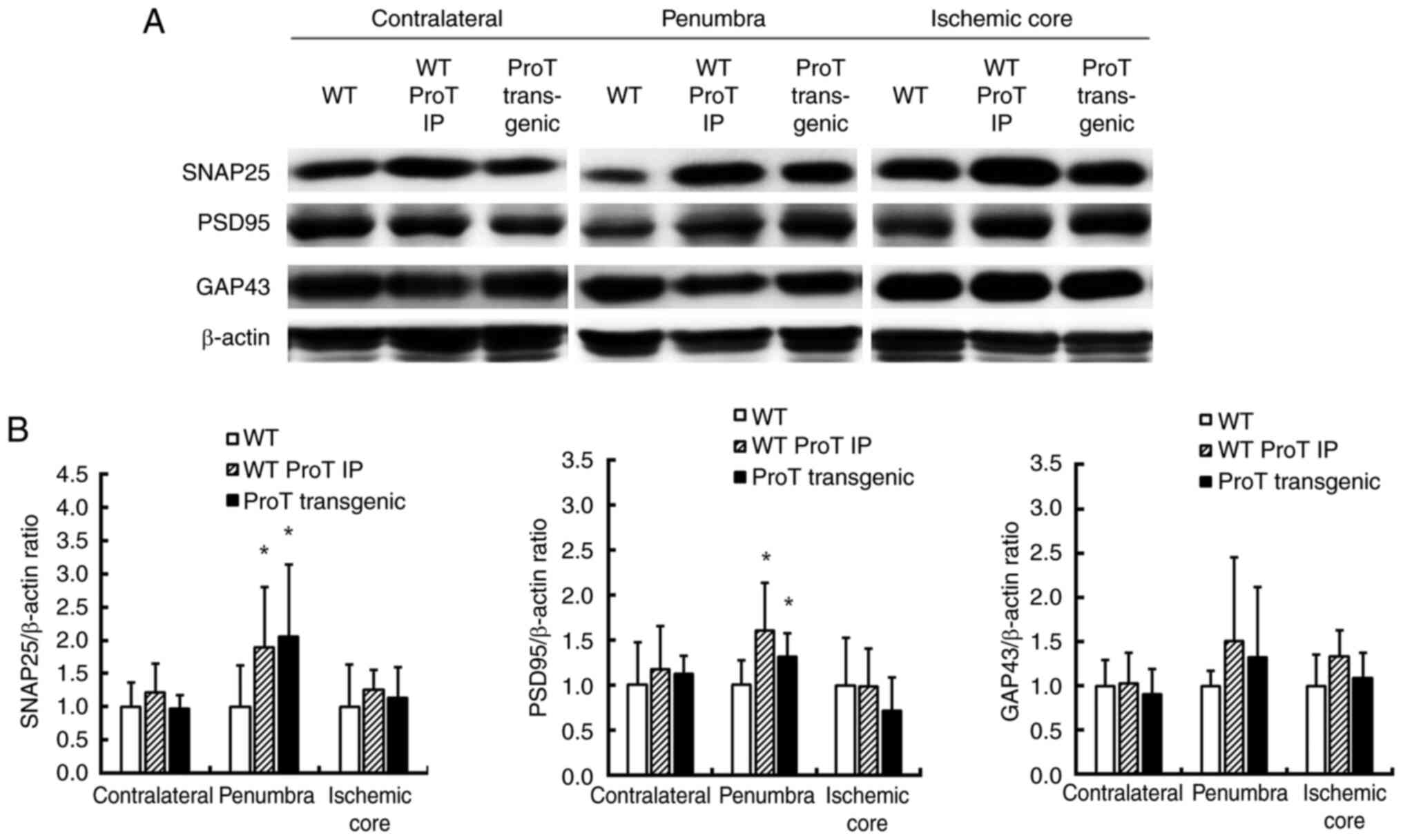
ProT increases neuroplasticity-associated proteins at the penumbra
SNAP-25 is a protein related to neuronal signal transmission. It primarily operates at presynaptic terminals, aiding in the regulation of neurotransmitter release, especially between neurons at synapses. The function of SNAP-25 is essential for normal neuronal transmission and it participates in inter-neuronal messaging (9,29). In presynaptic area analysis, SNAP-25 significantly increased in the ProT injection group and ProT overexpression in transgenic mice group compared with the control group at the penumbra (Fig. 6). However, there were no significant differences at the contralateral area and ischemic core. Concerning postsynaptic area analysis, PSD-95 is a protein located at the postsynaptic density of neurons and is typically involved in inter-neuronal signal transmission. It plays a crucial role at the postsynaptic density in regulating connections and communication between neurons. It is a synaptic protein that helps maintain the stability of neuronal connections (20,30). PSD-95 significantly increased in the ProT injection group and ProT overexpression in transgenic mice group compared with the control group at the penumbra. There was no significant difference between the contralateral area and the ischemic core.
Discussion
Stroke has attracted significant attention due to the high mortality rate and the effect on the lifestyle of stroke patients. The development of a good neuroprotectant is essential for clinical therapies. The present study demonstrated an increase in endogenous ProT expression following OGD injury. Previous reports have suggested that ProT is neuroprotective by preventing necrosis and apoptosis after stroke (13,14). However, the role of ProT in promoting neuroplasticity remains unclear.
The results of the present study indicated that ProT gene overexpression enhanced the length and dendritic branch recovery of neurites damaged by OGD toxicity. Having established the involvement of the ProT gene in neurite recovery, the present study proceeded to investigate the direct effects of ProT protein treatment. It revealed that ProT protein promoted neurite recovery, consistent with the transfection results. ProT possesses immunological functions at the nuclear localization signal (NLS), deleted in ProTΔNLS (31). A previous study reported that ProTΔNLS attenuates the proinflammatory activity and enhances the neuroprotective effects of ProT in ischemic injuries (18). Therefore, the present study also treated cells with ProTΔNLS through transfection and protein administration following OGD injury. The results indicated that ProTΔNLS also exerted neuroplasticity effects, but the improvement was not significantly better compared with ProT. Numerous studies have shown that ischemic stress induces a complete release of ProT in a serum- and supplement-free system (32–34). In serum-free conditions, neurons in low-density cultures undergo necrosis, while neurons cultured at high density exhibit an elevated ProT release, accompanied by increased apoptotic features and enhanced survival activity (35). When the conditioned medium from neurons in the high-density culture, which contained ProT, was added to the low-density culture, the survival activity markedly increased (35). In the present study, the neural cell culture medium initially contained serum and supplements, which were subsequently removed during the 2 h of OGD. The addition of ProT to the culture medium with serum and supplements resulted in a notable upregulation of BDNF mRNA expression and an increase in the cell survival rate.
A previous study mentioned that in vitro experiments on neurons cultured in hypoxic and low-glucose solutions, extracellular ProT changes the cell death mode from necrosis to apoptosis through putative Gi-coupled ProT receptor activation and delays neuronal cell death. During this period, neurotrophic factors, such as BDNF, are produced and inhibit apoptosis (36). BDNF plays an important role in neuronal survival and growth, serves as a neurotransmitter modulator and participates in neuronal plasticity (37). The current study demonstrated that the administration of ProT functions similarly to extracellular ProT, inducing an increase in BDNF mRNA expression. Therefore, to investigate the impact of ProT on neuronal plasticity, exploring neuroplasticity-related proteins associated with BDNF, such as GAP-43, PSD-95 and SNAP-25 (9,20,38), becomes crucial.
To further investigate the neuroplastic effect of ProT in vivo, the present study employed intra-arterial suture occlusion of the proximal right MCA on FVB wild-type mice and FVB ProT overexpression in transgenic mice in an animal model. The results demonstrated that ProT treatment or ProT overexpression in transgenic mice improved neurobehavioral outcomes compared with the control group, suggesting that ProT improves motor-sensory functional recovery following stroke. To investigate the molecular mechanism of the neuroplasticity effect of ProT after ischemic injury, the present study assessed the expression of several plasticity-associated proteins. The results revealed that ProT injection or the ProT overexpression in transgenic mice group exhibited increased expression of PSD-95 and SNAP-25, leading to improved neurite outgrowth and arborization. The expression of neuroplasticity-associated proteins were analyzed in three regions: Contralateral, penumbra and ischemic core. The contralateral area, corresponding to the healthy left brain, showed similar levels of plasticity-associated protein expression among the control group, ProT injection group and ProT overexpression in transgenic mice group. In the penumbra, ischemic damage is reversible through reperfusion and the levels of plasticity-associated proteins were significantly higher in the ProT injection and ProT overexpression in transgenic mice groups compared with the control group. However, no differences were observed in the ischemic core, where necrosis occurred.
Based on the aforementioned analysis and discussions, in conjunction with findings from previous studies and the results of the present study, it was concluded that ProT facilitated the enhancement of dendritic branch and length regrowth by increasing the expression of plasticity-associated proteins in vitro. Additionally, ProT treatment and ProT overexpression in transgenic mice resulted in less severe neurological behavioral outcomes following stroke. ProT treatment and ProT overexpression in transgenic mice exhibited increased protein levels of neuroplasticity-associated proteins compared with the control group. However, the detailed mechanism by which ProT promotes neuron regrowth remains unclear. It has been reported that deletion of the NLS from ProT decreases the expression of activated MMP-2 and MMP-9 72 h after ischemia/reperfusion injury (18). Another study has indicated that MMP enzymes also play essential roles in neuroplasticity and brain remodeling during the subacute stage of stroke (20,39,40). Further research is needed to elucidate these mechanisms.
Nevertheless, there are several potential limitations in the present study. First, although it demonstrated the potential positive effects of ProT on neuroplasticity following ischemia-reperfusion injury, it primarily focused on the cellular level and used mouse models. Further investigations are warranted in other animal models and clinical trials to determine the feasibility of applying ProT to human brain injuries. Second, the in vitro study used immunofluorescence staining to represent protein expression. For subsequent studies, alternative biotechnological assessments should be considered. Third, the present study predominantly concentrated on specific neuroplasticity-related proteins such as BDNF, SNAP-25 and PSD-95. However, neuroplasticity is a complex process regulated by various molecular mechanisms. Future investigations could expand to explore other related proteins and pathways to gain a more comprehensive understanding of ProT on neuroplasticity. Finally, the results of the present study were obtained in a controlled laboratory setting and real clinical situations may be more complex. Therefore, future research needs to consider the actual treatment conditions of patients to determine the clinical applicability of ProT and its potential limitations.
In conclusion, ProT is a promising neuroplasticity agent for treating ischemic stroke models in vitro and in vivo. The treatment of ProT in both gene transfection and protein addition increased the expression of neuroplasticity-associated proteins BDNF. In addition, ProT injection stroke mice and ProT overexpression in transgenic mice had a less severe outcome than the control group in the neurologic test. Furthermore, the expression of neuroplasticity-associated proteins PSD-95 and SNAP-25 increased at the penumbra area, indicating the repair and growth of ischemic damage neurons. The findings suggested that ProT has a potent neuroplastic effect in ischemic stroke. However, the detailed mechanism remains unclear. Further investigating ProT in developing novel therapy against ischemic stroke may be worthwhile.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was funded by a grant from the Ministry of Science and Technology of Taiwan, R.O.C. (grant no. MOST 109-2314-B-006-035).
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
Conceptualization was performed by EL and CW. ST and AL designed the experiments. The evaluation and confirmation of the experimental methodologies employed in the study were validated by ST. AL and SH analyzed and interpreted the data. EL AL and YC performed the experiments. Resources were from CW and EL. SH was responsible for data curation. AL and SH wrote the original draft. EL and CW wrote, reviewed and edited the manuscript. YC created figures, tables and visual representations of the data. CW and EL supervised the study. Project administration was done by LC. EL and AL confirm the authenticity of all the raw data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All procedures performed on experimental animals were approved by the Subcommittee on Research Animal Care of the National Cheng Kung University Medical Center (approval no. 109184).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Su F and Xu W: Enhancing brain plasticity to promote stroke recovery. Front Neurol. 11:5540892020. View Article : Google Scholar : PubMed/NCBI | |
|
Barone FC and Feuerstein GZ: Inflammatory mediators and stroke: New opportunities for novel therapeutics. J Cereb Blood Flow Metab. 19:819–834. 1999. View Article : Google Scholar : PubMed/NCBI | |
|
Clemens JA: Cerebral ischemia: Gene activation, neuronal injury, and the protective role of antioxidants. Free Radic Biol Med. 28:1526–1531. 2000. View Article : Google Scholar : PubMed/NCBI | |
|
Gürsoy-Ozdemir Y, Can A and Dalkara T: Reperfusion-induced oxidative/nitrative injury to neurovascular unit after focal cerebral ischemia. Stroke. 35:1449–1453. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
del Zoppo GJ: Stroke and neurovascular protection. N Engl J Med. 354:553–555. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Romero JR, Babikian VL, Katz DI and Finklestein SP: Neuroprotection and stroke rehabilitation: Modulation and enhancement of recovery. Behav Neurol. 17:17–24. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Legos JJ and Barone FC: Update on pharmacological strategies for stroke: Prevention, acute intervention and regeneration. Curr Opin Investig Drugs. 4:847–858. 2003.PubMed/NCBI | |
|
Bang OY, Kim EH, Cha JM and Moon GJ: Adult stem cell therapy for stroke: Challenges and progress. J Stroke. 18:256–266. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Chen HY, Hung YC, Chen TY, Huang SY, Wang YH, Lee WT, Wu TS and Lee EJ: Melatonin improves presynaptic protein, SNAP-25, expression and dendritic spine density and enhances functional and electrophysiological recovery following transient focal cerebral ischemia in rats. J Pineal Res. 47:260–270. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Freire M, Sarandeses CS, Covelo G and Díaz-Jullien C: Phosphorylation of prothymosin α. An approach to its biological significance. Vitam Horm. 102:73–99. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Fujita R, Ueda M, Fujiwara K and Ueda H: Prothymosin-alpha plays a defensive role in retinal ischemia through necrosis and apoptosis inhibition. Cell Death Differ. 16:349–358. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Teixeira A, Yen B, Gusella GL, Thomas AG, Mullen MP, Aberg J, Chen X, Hoshida Y, van Bakel H, Schadt E, et al: Prothymosin α variants isolated from CD8+ T cells and cervicovaginal fluid suppress HIV-1 replication through type I interferon induction. J Infect Dis. 211:1467–1475. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Fujita R and Ueda H: Prothymosin-alpha1 prevents necrosis and apoptosis following stroke. Cell Death Differ. 14:1839–1842. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Ueda H: Prothymosin alpha plays a key role in cell death mode-switch, a new concept for neuroprotective mechanisms in stroke. Naunyn Schmiedebergs Arch Pharmacol. 377:315–323. 2008. View Article : Google Scholar : PubMed/NCBI | |
|
Karapetian RN, Evstafieva AG, Abaeva IS, Chichkova NV, Filonov GS, Rubtsov YP, Sukhacheva EA, Melnikov SV, Schneider U, Wanker EE and Vartapetian AB: Nuclear oncoprotein prothymosin alpha is a partner of Keap1: Implications for expression of oxidative stress-protecting genes. Mol Cell Biol. 25:1089–1099. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Ueda H: Prothymosin alpha and cell death mode switch, a novel target for the prevention of cerebral ischemia-induced damage. Pharmacol Ther. 123:323–333. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Halder SK, Sugimoto J, Matsunaga H and Ueda H: Therapeutic benefits of 9-amino acid peptide derived from prothymosin alpha against ischemic damages. Peptides. 43:68–75. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Wang LC, Wu CL, Cheng YY and Tsai KJ: Deletion of nuclear localizing signal attenuates proinflammatory activity of prothymosin-alpha and enhances its neuroprotective effect on transient ischemic stroke. Mol Neurobiol. 54:582–593. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Belayev L, Alonso OF, Busto R, Zhao W and Ginsberg MD: Middle cerebral artery occlusion in the rat by intraluminal suture. Neurological and pathological evaluation of an improved model. Stroke. 27:1616–1623. 1996. View Article : Google Scholar : PubMed/NCBI | |
|
Juan WS, Huang SY, Chang CC, Hung YC, Lin YW, Chen TY, Lee AH, Lee AC, Wu TS and Lee EJ: Melatonin improves neuroplasticity by upregulating the growth-associated protein-43 (GAP-43) and NMDAR postsynaptic density-95 (PSD-95) proteins in cultured neurons exposed to glutamate excitotoxicity and in rats subjected to transient focal cerebral ischemia even during a long-term recovery period. J Pineal Res. 56:213–223. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Lee EJ, Wu TS, Lee MY, Chen TY, Tsai YY, Chuang JI and Chang GL: Delayed treatment with melatonin enhances electrophysiological recovery following transient focal cerebral ischemia in rats. J Pineal Res. 36:33–42. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Li KJ, Shiau AL, Chiou YY, Yo YT and Wu CL: Transgenic overexpression of prothymosin alpha induces development of polycystic kidney disease. Kidney Int. 67:1710–1722. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Su BH, Tseng YL, Shieh GS, Chen YC, Shiang YC, Wu P, Li KJ, Yen TH, Shiau AL and Wu CL: Prothymosin α overexpression contributes to the development of pulmonary emphysema. Nat Commun. 4:19062013. View Article : Google Scholar : PubMed/NCBI | |
|
Huang SY, Chang CH, Hung HY, Lin YW and Lee EJ: Neuroanatomical and electrophysiological recovery in the contralateral intact cortex following transient focal cerebral ischemia in rats. Neurol Res. 40:130–138. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Bederson JB, Pitts LH, Tsuji M, Nishimura MC, Davis RL and Bartkowski H: Rat middle cerebral artery occlusion: Evaluation of the model and development of a neurologic examination. Stroke. 17:472–476. 1986. View Article : Google Scholar : PubMed/NCBI | |
|
Clark WM, Rinker LG, Lessov NS, Hazel K, Hill JK, Stenzel-Poore M and Eckenstein F: Lack of interleukin-6 expression is not protective against focal central nervous system ischemia. Stroke. 31:1715–1720. 2000. View Article : Google Scholar : PubMed/NCBI | |
|
Caceres A, Banker G, Steward O, Binder L and Payne M: MAP2 is localized to the dendrites of hippocampal neurons which develop in culture. Brain Res. 315:314–318. 1984. View Article : Google Scholar : PubMed/NCBI | |
|
DeGiosio RA, Grubisha MJ, MacDonald ML, McKinney BC, Camacho CJ and Sweet RA: More than a marker: Potential pathogenic functions of MAP2. Front Mol Neurosci. 15:9748902022. View Article : Google Scholar : PubMed/NCBI | |
|
Tomasoni R, Repetto D, Morini R, Elia C, Gardoni F, Di Luca M, Turco E, Defilippi P and Matteoli M: SNAP-25 regulates spine formation through postsynaptic binding to p140Cap. Nat Commun. 4:21362013. View Article : Google Scholar : PubMed/NCBI | |
|
Yoo KS, Lee K, Oh JY, Lee H, Park H, Park YS and Kim HK: Postsynaptic density protein 95 (PSD-95) is transported by KIF5 to dendritic regions. Mol Brain. 12:972019. View Article : Google Scholar : PubMed/NCBI | |
|
Skopeliti M, Iconomidou VA, Derhovanessian E, Pawelec G, Voelter W, Kalbacher H, Hamodrakas SJ and Tsitsilonis OE: Prothymosin alpha immunoactive carboxyl-terminal peptide TKKQKTDEDD stimulates lymphocyte reactions, induces dendritic cell maturation and adopts a beta-sheet conformation in a sequence-specific manner. Mol Immunol. 46:784–792. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Ueda H: Non-vesicular release of alarmin prothymosin α complex associated with annexin-2 flop-out. Cells. 12:15692023. View Article : Google Scholar : PubMed/NCBI | |
|
Ueda H, Fujita R, Yoshida A, Matsunaga H and Ueda M: Identification of prothymosin-alpha1, the necrosis-apoptosis switch molecule in cortical neuronal cultures. J Cell Biol. 176:853–862. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Matsunaga H and Ueda H: Stress-induced non-vesicular release of prothymosin-α initiated by an interaction with S100A13, and its blockade by caspase-3 cleavage. Cell Death Differ. 17:1760–1772. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Fujita R, Yoshida A, Mizuno K and Ueda H: Cell density-dependent death mode switch of cultured cortical neurons under serum-free starvation stress. Cell Mol Neurobiol. 21:317–324. 2001. View Article : Google Scholar : PubMed/NCBI | |
|
Ueda H: Prothymosin α plays role as a brain guardian through Ecto-F1 ATPase-P2Y12 complex and TLR4/MD2. Cells. 12:4962023. View Article : Google Scholar : PubMed/NCBI | |
|
Huang EJ and Reichardt LF: Neurotrophins: Roles in neuronal development and function. Annu Rev Neurosci. 24:677–736. 2001. View Article : Google Scholar : PubMed/NCBI | |
|
Tai SH, Huang SY, Chao LC, Lin YW, Huang CC, Wu TS, Shan YS, Lee AH and Lee EJ: Lithium upregulates growth-associated protein-43 (GAP-43) and postsynaptic density-95 (PSD-95) in cultured neurons exposed to oxygen-glucose deprivation and improves electrophysiological outcomes in rats subjected to transient focal cerebral ischemia following a long-term recovery period. Neurol Res. 44:870–878. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Michaluk P, Wawrzyniak M, Alot P, Szczot M, Wyrembek P, Mercik K, Medvedev N, Wilczek E, De Roo M, Zuschratter W, et al: Influence of matrix metalloproteinase MMP-9 on dendritic spine morphology. J Cell Sci. 124:3369–3380. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Oliveira-Silva P, Jurgilas PB, Trindade P, Campello-Costa P, Perales J, Savino W and Serfaty CA: Matrix metalloproteinase-9 is involved in the development and plasticity of retinotectal projections in rats. Neuroimmunomodulation. 14:144–149. 2007. View Article : Google Scholar : PubMed/NCBI |